I have a toddler.
Whenever I take him to his paediatrician, I carry a big folder containing all his ‘paper’ records. Records that got handed over to me from the time he was born all the way to the last vaccine he was administered. The folder also contains all the paper bills, prescriptions, immunisation records, and everything else. Sometimes, I forget to file certain prescriptions, and sometimes, the vaccination entry that his paediatrician made on the vaccination card gets smudged because it was written with ink that hates water. India experiences heavy monsoons, and sometimes ‘paper’ records get wet. I hold onto that folder like it is the most important thing in my life.
It probably is.
If it gets lost, I will not only lose my kid's entire medical history but also probably impact his future medical interventions since healthcare is contextual and context is locked in that paper.
Now, my parents - well, that’s a different story. They are a happier bunch. When I asked them if they knew their vaccination schedule when they were kids, they laughed it off, firmly believing I had nothing better to do than ask these irrelevant questions. I asked them if they remembered if ‘my’ vaccination schedule was followed as expected, and they thought long and hard. The ending of that thought was inconclusive.
I can only thank the universe for how far we have come from where we were to where we are now. We at least have records.
Paper records …..
It is time to raise our game now.
We have already produced a lot of medical data over the course of our lifetime. That data is sitting in a computer of some clinic or a hospital, or a lab. This data is worth its weight in gold because it has captured snapshots of our health over a period of time and has context that has a direct bearing on our longevity, productivity and, most importantly, our happiness. And yet, we ignore it because there is no easy way to connect the dots. Imagine if only there were a way to connect all that data across various health entities captured across years and extract insights and information from it.
Enter Ayushman Bharat Digital Mission (ABDM).
Why is this mission important for India?
The litmus test of any Health system is how well it caters to the Iron Triangle of Healthcare - Access, Cost, and Quality.
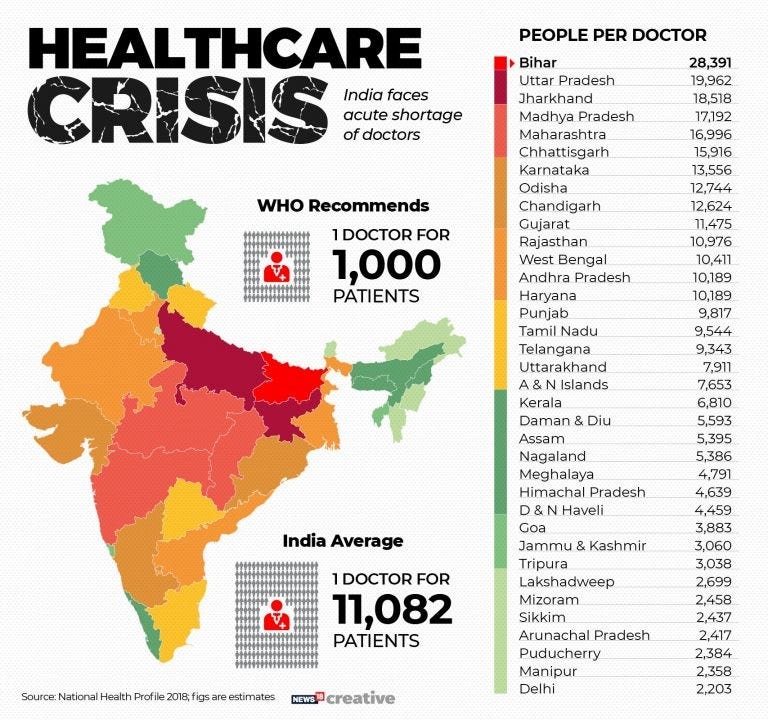
Healthcare is one of any country's most important focus areas, let alone a country with such a young population yielding an unparalleled demographic dividend. India has over 600,000 villages, 121 languages and 19500 dialects. With a large and diverse population, it almost becomes a moral obligation for the country to cater to the Iron Triangle. But can it? India still has less than 1 doctor per 1,000 people, which is lower than the WHO recommended ratio of 1 per 1000. There are over 1.2 Million doctors, and even with ~50,000 fresh graduates coming out of med schools every year, India will take some time to reach the WHO recommended ratio. Another issue is that 70% of the medical infrastructure is concentrated in urban India while only 35% population lives there - more than 65% of India is NOT urban. This in itself is a challenge when it comes to keeping a country this big and healthy. In addition, around 5 - 6 crore Indians are pushed into poverty every year because of a medical event that they cannot bear the cost of. That is roughly 4.5% of the nation pushed into poverty year after year. This certainly is not an ideal state for any country to be in.
Source: CNBC TV18
Now, there are some levers you can pull, like increasing the supply of doctors, beds, hospitals, etc., but as you may realise, this is more challenging than it sounds and will take significant time. But there is one easy lever to pull: optimising the existing capacity.
When you look up a new doctor and see that this person has 800 reviews averaging 2 stars, would you visit him even if their rates are the cheapest in your area?
Now consider another scenario where a ‘Teleconsult’ costs you twice as much, but you clearly see that this doctor has 800 reviews averaging to 4.8 stars. Will you consider this doctor over the other?
Exactly.
This in HealthTech parlance, especially ABDM, is called ‘discoverability’. Discoverability changes everything.
In a low-resource setting like ours, digital is that light at the end of the tunnel.
The ‘Digital Public Goods’ approach ABDM takes has a higher likelihood of success.
For the uninitiated, ‘public goods’ are goods built for the public and are non-excludable and non-rival.
Non-excludable = nobody can be excluded from using those public goods
Non-rival = consumption of those goods by some does not decrease the supply for others
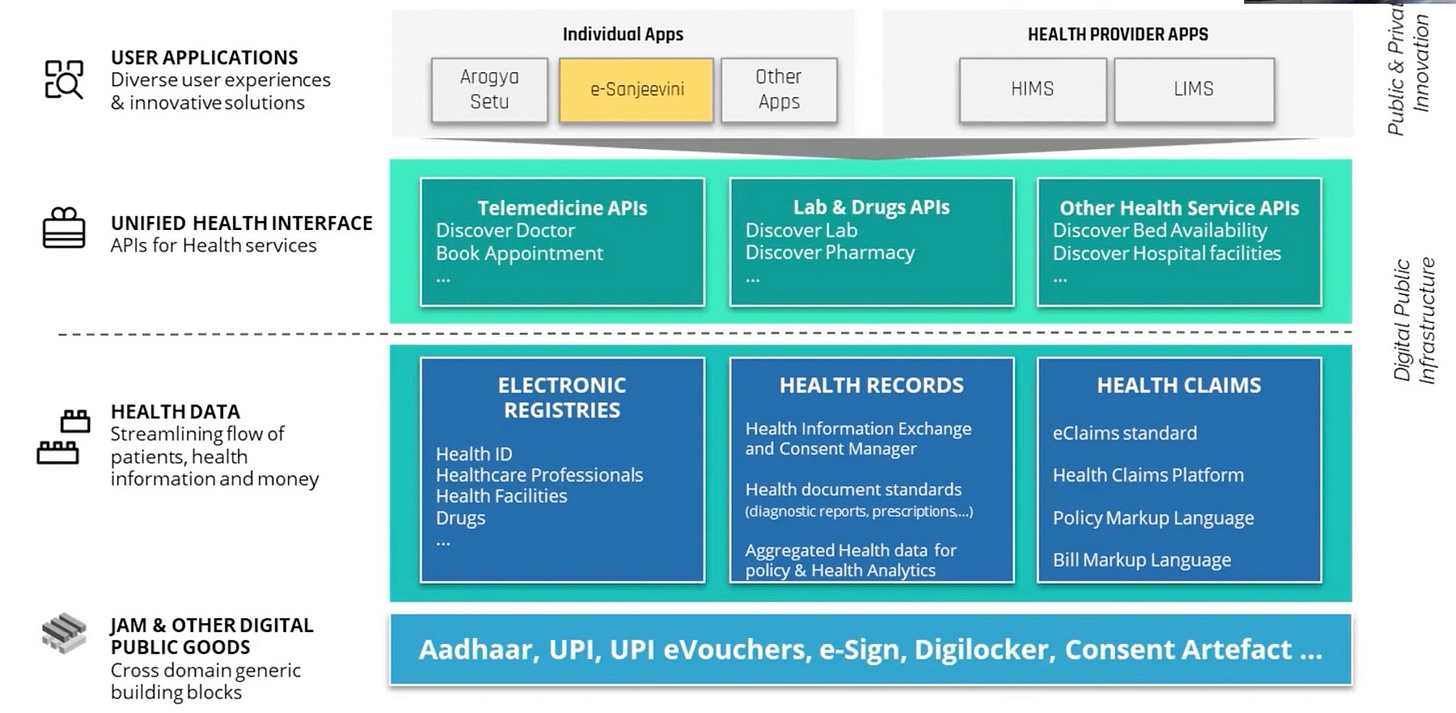
A classic example of such a digital public good that millions of Indians used in the recent past is Cowin. Everybody could access the website to book vaccination appointments; no one was excluded, and someone accessing it did not stop someone else from accessing it. What is interesting to note here is that Cowin already used one of the building blocks of the ABDM - Healthcare Facilities registry. When you logged into Cowin to book your vaccination slot, you saw a list of healthcare facilities where the vaccinations were administered- public and private. That list came from the National Health Stack, architecture built to cater to ABDM.
Source: Screen grab from NHA YT channel
But before diving more into the National Health Stack, it is obligatory to understand its predecessor - India Stack - where it all started…..
Source: iSpirt - India Stack
What you see above is basically an architectural representation of India Stack - a set of open APIs and digital public goods that aim to unlock the economic primitives of identity, data, and payments at the population scale. This is basically the architecture on top of which all the initiatives like Adhaar, DigiLocker, Digital KYC, etc, are built. When the current government first came to power in 2014, it made a big push for the use of technology catering to the financial inclusion of the underserved. The Jan Dhan - Adhaar - Mobile (JAM) trinity was proposed in the Economic Survey of 2014-2015. It did 2 main things - it really pushed the mobile agenda. It laid the foundation for a Unified Payment Interface, which would become so ubiquitous 6 years later that everyone from my vegetable vendor to high-end restaurants today prefers UPI-based payment over cash, given the convenience. India’s per person per month data consumption is about 12 GB today, expected to increase to 25 GB by 2025. This is the highest consumption globally. Around 1 billion Indians will be on smartphones by 2025. Over 1 billion Indians already have their Adhaar ID, which is a 12-digit unique identity provided by the Unique Identification Authority of India (UIDAI). This ID has already become a significant part of everybody’s lives. It is safe to assume that India is comfortable with digital.
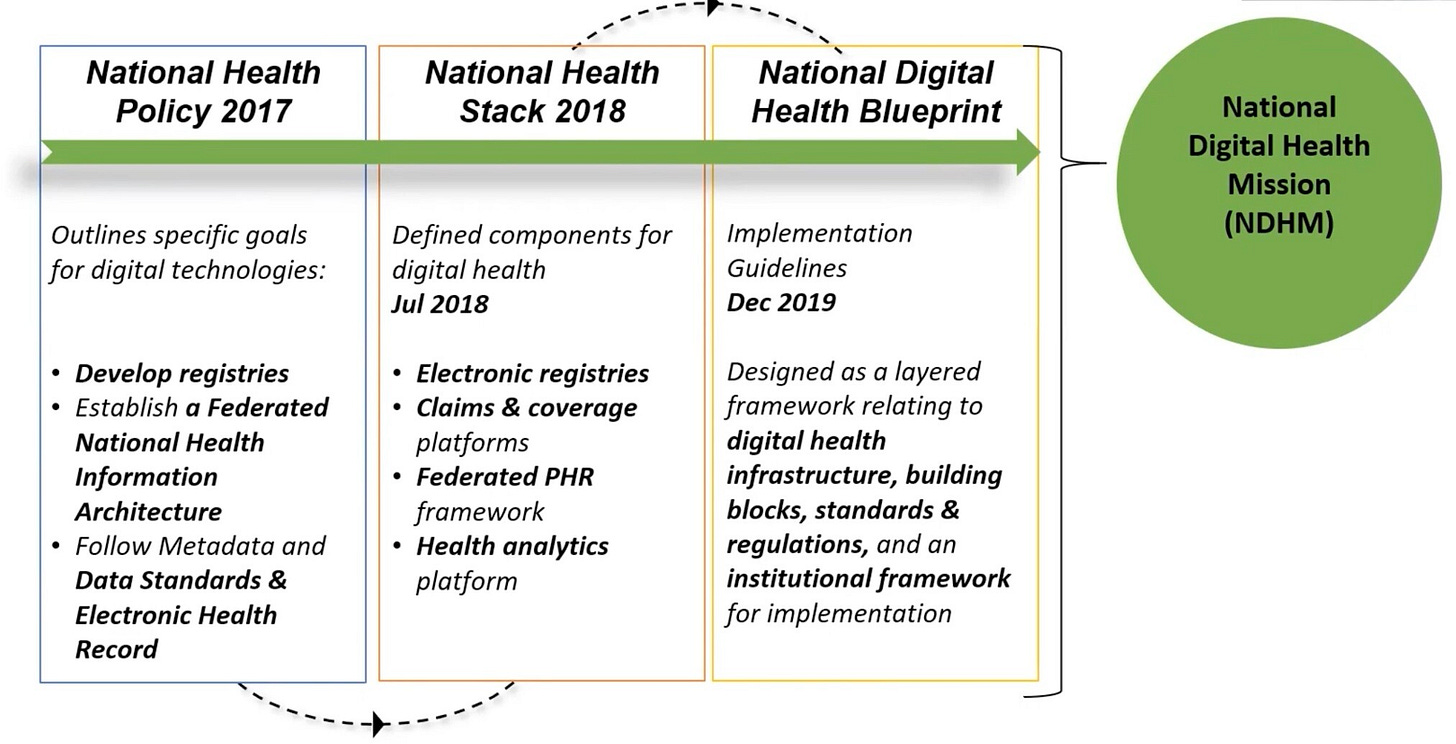
Now, coming back to the National Health Stack - it is modelled roughly along the same lines as the India Stack. The National Health Authority (NHA) has also laid out a comprehensive vision of what it intends to accomplish via the open architecture it has conceived. It intends to power through the building blocks - as many as possible - and then leave the innovation to private players.
Source: National Health Authority(NHA)
What started as an idea regarding India Stack as a Digital Public Good is today a powerhouse on which billion-dollar companies like Paytm were founded. The government built the infrastructure and let the private companies innovate. The way I look at it is that the government already has a digital public goods playbook in terms of India Stack, which it now intends to replicate in the form of the National Health Stack, and I hope that the industry responds the same way it did the first time.
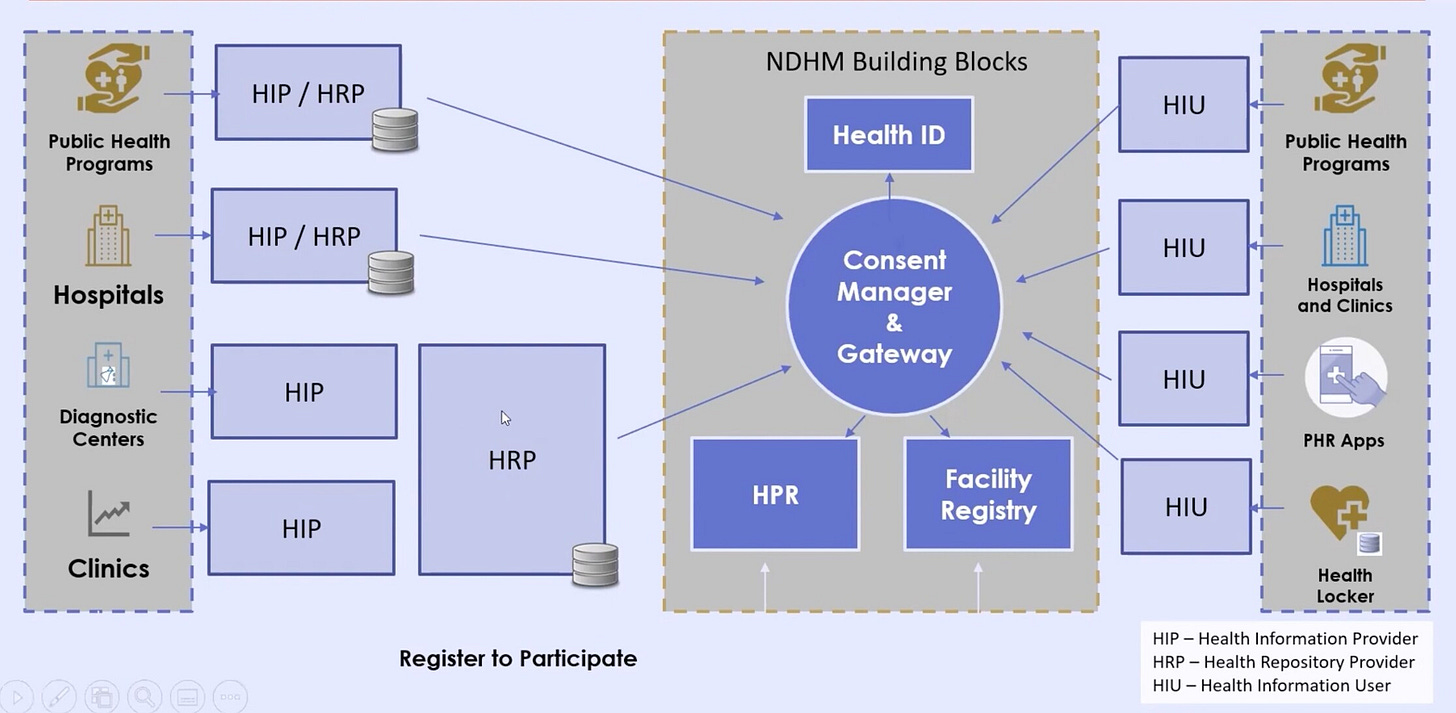
Federated and consent-based architecture is a progressive paradigm.
I read a lot of articles about how NHA will store all this health data, and there is a strong chance that it may get exploited by bad actors. Some even raised alarms that this was a national security issue. But before we go too far with this train of thought, it is important to understand the ‘federated architecture’ that NHA has proposed. As you see below, NHA is not going to store any data. The responsibilities are distributed at the national, state and local levels. At the national level, the government will only ensure that all the critical building blocks are developed and maintained as expected. This includes the health professionals registry, the health facility registry and other items critical to the smooth functioning of the eco-system. It is leaving other responsibilities to the state and local levels. Basically, your data that currently sits on the servers of healthcare facilities you have voluntarily visited will not move - unless you consent.
Source: abdm.gov.in
As you see below, all arrows point to a ‘consent manager’ - which is basically a good thing. A consent manager is a module that sits between the two entities trying to exchange your medical data.
So, how does consent management work?
If you were to visit a hospital in Maharashtra and then move to Delhi and now try to visit a hospital in Delhi that requires some of your records from the hospital in Maharashtra, it can - via the ABDM workflow - send a request to get specific records. Now, because this request is based on your health ID, which is mapped to you, a ‘consent request’ comes to you via the health app you are using. The consent request clearly states what are the specific records being requested by the hospital in Delhi. You can set an approval window for the consent, after which the consent expires, and the hospital in Delhi has to delete your data. Once you hit approve, the data flows outside of the ABDM framework directly between the 2 hospitals.
Source: YT screengrab from NATHEALTH
The federated architecture and consent management workflow enhance the trust quotient of the overall initiative, thus enabling higher confidence in sharing data, eventually helping in higher-quality decision-making.
Interoperability standards that enable true health data liquidity are at the centre of the ABDM universe.
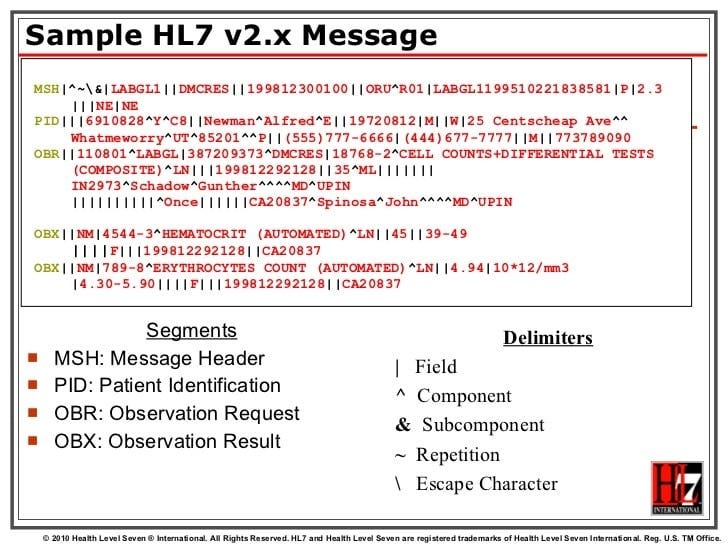
I have spent over a decade analysing the US HealthTech ecosystem. One of the first professional certifications I worked towards was HL7 v2.X. Health Level Seven (HL7) is an international standards body at the centre of creating such interoperability standards. It all started with HL7 version 2 (HL7 v2). HL7 v2 is basically a standard to exchange your health information (in an antiquated way) and is widely adopted across most interoperability workflows in the US, even today. All major software vendors support this standard. This is how a sample v2.x message looks and what do some of the things included in there mean.
Source: HL7
You would be surprised that this standard was created in 1989. So, a standard that was created 3 decades back still manages to hold the lion’s share of interoperability for reasons way beyond the premise of this article. The bottomline is that HL7 v2 kicked open the doors of interoperability. It then evolved into various standards, as all good standards should.
V3 Messaging Standard – an interoperability specification for health and medical transactions
Clinical Document Architecture (CDA) – for clinical documents, based on HL7 Version 3
Continuity of Care Document (CCD) – for exchange of medical summaries based on CDA.
Although all the standards above served their purpose, they were not ‘internet friendly’ in some ways. Parsing them and consuming the underlying information came at a cost. HL7 now has a brand new interoperability standard to support modern web architecture, basically. It is called FHIR - Fast Healthcare Interoperability Resources. It is a standard based on RESTful web services and supports JSON. And because it is developer-friendly, it cuts down a lot of implementation time and has a higher likelihood of adoption and, thereby, survival in the long run.
RS Sharma - CEO of the National Health Authority, recently said, and I agree, that in HealthTech - ‘not having a legacy is a blessing’. While many of the US are still stuck on HL7 v2.X, India went straight to FHIR given the ubiquity. Standards bring ‘structure’ to health data, which makes that data valuable since it has rich downstream uses. ABDM has done an impressive job at - first of all, choosing to follow standards - and then picking modern ones. Consider standards as basically being ‘languages’ in which Health systems talk to each other. If two systems implement a common standard (read or speak the common language) - they understand each other. God saves them (and us) if they have not implemented any standard.
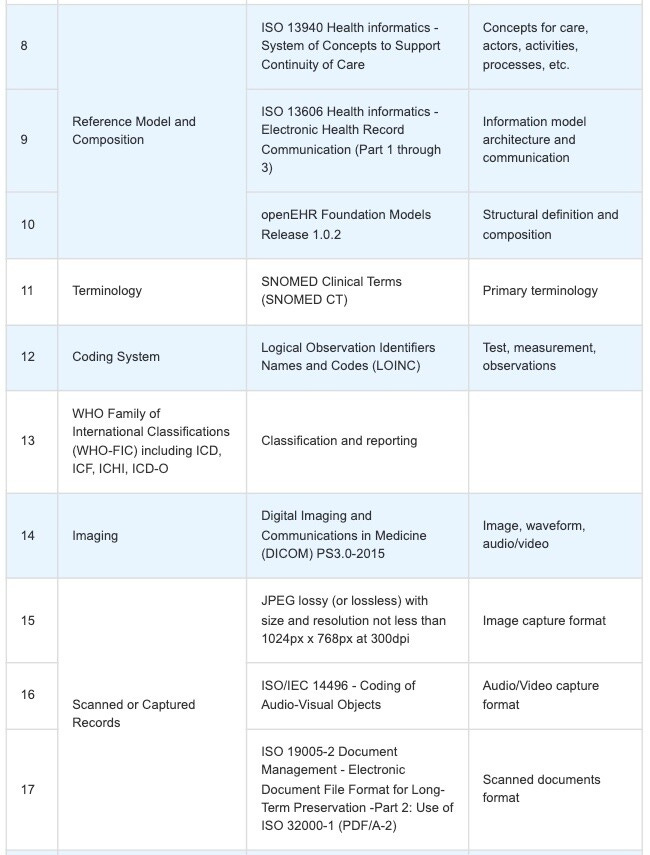
I was pleasantly surprised to see a comprehensive list of standards that have made the roster of ABDM. LOINC for labs, DICOM for imaging, etc., indicate a HealthTech eco-system moving in the right direction. And I have picked up only half of what’s on the list. You can find the remaining half here.
Source: NHP.gov
5 probable reasons why ABDM might fail
Carl Jacobi famously said - ‘Invert, always invert’. So invert we should.
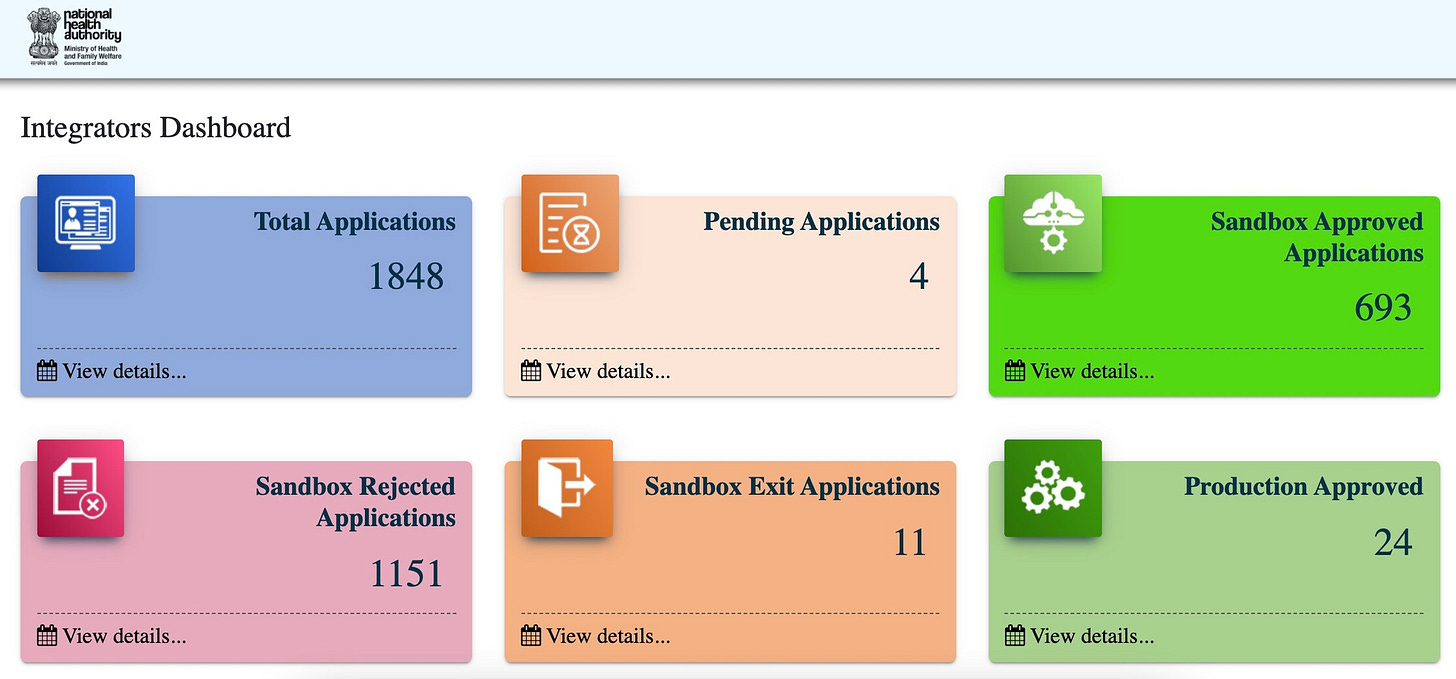
ADBM has a couple of failure modes. The biggest one is that it is ‘voluntary’ in nature. There is no law at the moment mandating participation. One of the primary aspects of this mission, which is not very apparent, is that for any health entity to send data to any other health entity, it must be ‘integrated’ with the ABDM eco-system. ABDM has made this really easy by floating SOPs on how to integrate here. India has over 65,000 hospitals, 110,000 labs, and 850,000 retail pharmacies, amongst other facilities providing some form of care to patients. 6 million OPD visits happen daily. Imagine what happens if most health entities ignore the ABDM pitch. The entire initiative falls apart.
Integration is the rate-limiting factor.
ABDM maintains a comprehensive dashboard of all the entities that are attempting to integrate and their integration status. As of Dec 22nd, 2021, that dashboard looked like what you see below. Notice that only 24 entities are ‘Production approved’, which in layman's terms means that only 24 entities can currently exchange health data of patients who visited them with each other at the moment. This is nothing compared to the numbers we just discussed. So, there has to be a concerted effort from the NHA to engage with the broader industry to build awareness around the integration, understand the roadblocks and then remove them.
Source: ABDM Sandbox environment
ABDM architecture currently allows multiple PHR addresses via multiple consent managers, and that could soon spiral out of control
The ABDM PHR address, which looks something like yourname@ndhm, is at the centre of your health data exchange. This address will be tied to a consent manager to manage consent for a particular request around accessing your health information. The problem is that there can be multiple such addresses since there can be various such consent managers. Nothing in the overall architecture restricts it. The obvious downside is that if I sign up with 2 or more consent managers via their Health App and have 2 or more PHR addresses, I really need a third-party app to map all these PHR addresses back to me.
How will this third-party app manage consent from two or more different consent managers if all the data will be in sync all the time and more such questions are outside this discussion? The fact of the matter is that if you have multiple PHR addresses that need to be appropriately linked in all your health systems that store your health data, things spiral out of control very quickly, and you will lose the audience.
The entire consent management workflow being socialised now is geared more towards smartphones.
All the NHA presentations I have attended till now talk about the consent request coming to your ‘smartphone’. Just 2 years back, about 400 million people were still using feature phones - basically, phones that do not have touch screens. If we want to cater to ‘access’, we better understand that someone who does not have access to healthcare is probably not using smartphones. So the obvious next step is to consider bringing those 400 Mn feature phone users into the fold of consent management and, thereby, ABDM.
Disinterested doctors
Given the load on doctors, they are generally so overwhelmed that they need more time to do anything besides what they should be doing- treating patients. Not all doctors have assistants who can manage administrative tasks. Not all doctors are well-versed with computers. Not all doctors are interested in technology even. I would argue that most doctors want to avoid this unless they see the value. It is thus imperative that ABDM does effective outreach that can help doctors really become interested in participating in the initiative and make that tangible difference,
Tight coupling with English/Hindi as primary languages
All the outreach, without exception, is in either English or Hindi. Check it out for yourself. The Indian Constitution even has a mention of 22 languages. We need to include the remaining 20 major languages. So that you know, I am completely ignoring the 19000 dialects here. Only 44% of the population speaks Hindi. 8% speak Bengali, 7% speak Telugu, 6% Tamil, etc. Do we really want to ignore the remaining 50% of the country in this most critical outreach? We should start going multi-lingual on all platforms if we want to move the needle here.
Having analysed the failure modes, one thing is sure: the NHA is definitely not winging it. Ayushman Bharat Digital Mission has some of the Tech industry’s brightest brains behind it. Not just that, it also has comprehensive guidance and detailed technical documentation available on abdm.gov.in. The NHA has published several consultation papers on the critical building blocks of the National Health Stack, soliciting comments from the industry and has incorporated the feedback wherever appropriate. And and and ……. it has made available what is every IT guy’s dream - a sandbox environment where it has published in detail the architecture, APIs and standards around how to integrate and play around with this eco-system. ‘Good Health & well-being’ is one of the 17 sustainable development goals the United Nations set to make our future more sustainable. Ayushman Bharat Digital Mission is India’s bold response to accelerate that vision. I strongly feel that the winds are blowing in the right direction, and the Indian health system has a good chance of leapfrogging some of the advanced systems if things land as expected.
So, while ABDM may have its sceptics, I am betting my money on its success today.








This is such a fabulous article! Hope to read your thoughts again later as NHA's broad vision unfolds over the years.