HL7® v2.x: The 800-pound gorilla in the Interoperability room
The rain was relentless, each droplet seemingly in a race to hit the ground. I was on my bike with my raincoat on. My mind was preoccupied as I manoeuvred through the busy streets of Powai (Mumbai), dodging puddles and incessant honking. Auto rickshaws darted around with their characteristic assertiveness, rarely yielding space. But having grown up amidst this chaos, I knew better. I managed to navigate successfully to reach my destination. The occasion for this heroic film-like sequence, you ask?
HL7® certification exam.
I stumbled upon the examination hall after what felt like an eternity. The ambience inside was a stark contrast to the chaos outside. A few scattered souls, each engrossed in their thoughts, awaiting the challenge ahead. Only a select few in India, and even globally, attempt the certification - so the whole experience felt very exclusive. I was inadvertently placing myself in a small group of HL7® domain experts.
While the exam format, the questions, and the pressure are all exciting things, that’s not what I want to discuss.
Today, I want to talk about the specific standard for which I was attempting that certification exam, the 800-pound gorilla of interoperability standards - HL7® v2.x.
Diving into the Layers of HealthTech Interoperability
Imagine you're travelling to a foreign country.
You're immediately surrounded by unfamiliar sounds and sights as you step off the plane. To navigate this new environment, you'll need two essential tools: a basic understanding of the local language (the words and their order) and a grasp of the cultural nuances behind specific phrases or gestures. This is how you exchange information. Exchanging healthcare information is no different. There are 2 broad categories of interoperability.
Syntactic Interoperability: Think of syntax as the order of words in a sentence. It's the rules of grammar that dictate how sentences are formed. For instance, the typical sentence structure in English is subject-verb-object, as in "I love music." In HealthTech, syntax refers to the standardised format or structure in which data is exchanged between systems. It ensures all parties use the same "grammar" when transmitting information. In HL7® v2.x, messages are structured in segments, each representing a specific data type.
Here is a sample HL7® v2.x message with placeholder patient information.
MSH|^~\&|SENDING_APPLICATION|SENDING_FACILITY|RECEIVING_APPLICATION|RECEIVING_FACILITY|202307051028||ORU^R01|102807|P|2.
PID|||123456||DOE^JOHN||19700101|M|||123 MAIN ST^^ANYTOWN^OH^12345||(555)555-5555|||M
OBX|1|TX|LocalCode1^BP||120/80|||N
OBX|2|TX|LocalCode2^Temp||98.6|F|||NThe MSH "segment" is the message header, providing metadata about the message, and the PID segment contains patient identification details. Each field is separated by a delimiter ("|" pipe in this case). Any system that understands HL7® v2.x can interpret this message correctly because it follows the "grammar" rules set by the HL7® v2.x standard. This is how HL7® v2.x aids in achieving syntactic interoperability, ensuring that healthcare systems use a standard structure or format when they exchange data.
But what "BP" and "Temp" mean to one facility may not mean the same to another facility. And this is where semantic interoperability comes into the picture.
Semantic Interoperability: Once you've understood the syntax of a language, there's another layer of complexity: semantics, or the meaning behind all those words and phrases. For example, "biscuit" has different meanings in the UK and the US. In the UK, it refers to a sweet snack similar to what Americans call a "cookie," whereas, in the US, it typically refers to a soft bread item. In healthcare, semantics ensures that terms are universally understood. It's not enough for two systems to exchange the word "BP"; both must also agree on whether it stands for "blood pressure" or "bipolar."
Standards like SNOMED CT help in semantic interoperability, ensuring that medical terms are consistently interpreted across healthcare facilities.
How, you ask?
SNOMED CT is a comprehensive clinical terminology system; medical terms are assigned unique codes to ensure consistent interpretation across healthcare facilities. Let us revisit the sample HL7® v2.x message above with actual SNOMED CT codes for systolic, diastolic and body temperature.
MSH|^~\&|SENDING_APPLICATION|SENDING_FACILITY|RECEIVING_APPLICATION|RECEIVING_FACILITY|202307051028||ORU^R01|102807|P|2.
PID|||123456||DOE^JOHN||19700101|M|||123 MAIN ST^^ANYTOWN^OH^12345||(555)555-5555|||M
OBX|1|NM|271649006^Systolic blood pressure^SNOMED-CT||120|mmHg|||N
OBX|2|NM|271650006^Diastolic blood pressure^SNOMED-CT||80|mmHg|||N
OBX|3|NM|386725007^Body temperature^SNOMED-CT||98.6|F|||N3The OBX segments now use SNOMED CT codes to represent the observations in this standardised message. If you play around with the freely accessible SNOMED CT browser, you'll realise that
271649006 means "Systolic blood pressure"
271650006 means "Diastolic blood pressure"
386725007 means "Body temperature"
Assuming the receiving system has also implemented SNOMED CT, it can unambiguously understand the meaning of this information. This code ensures that when healthcare systems across the globe refer to "Blood Pressure," they all refer to the same concept, thereby achieving semantic interoperability even globally. Together, these two layers ensure that when healthcare systems communicate, they speak the same language and understand the meaning of the data being exchanged in that language.
According to a study by Johns Hopkins, 44 per cent of medical error deaths are preventable by implementing advanced interoperability solutions. The bottomline is that interoperability is not just about coding systems and syntaxes; it saves lives!
The Critical Role of Interoperability in Modern Healthcare
"Healthcare is not a solo act. It really is a whole orchestra doing jazz 24/7 for a population of 330 million people."
Aaron Seib, Senior Vice President of Strategy and Innovation, NewWave (US).
Great analogy. Let's take it further. So if healthcare is an orchestra, who's the conductor?
Interoperability.
Like the conductor who seamlessly blends the powerful brass, delicate strings, and rhythmic percussion into a harmonious melody, interoperability orchestrates the information flow between myriad healthcare systems. It ensures that each 'instrument'—from patient records to diagnostic tools—plays in tune, synchronising their outputs to create a cohesive and holistic patient care symphony.
The Essence of Patient-Centric Care: Every individual's health journey is a unique narrative, filled with chapters of wellness, illness, recoveries, and milestones. Interoperability ensures that each chapter, written in a city hospital or a rural clinic, seamlessly blends into the next. This continuity paints a complete picture, allowing caregivers to tailor their approach and ensuring every patient feels heard, understood, and cared for.
Achieving Operational Harmony: Beyond patient narratives, healthcare is a symphony of operations. Every process has its tempo, from the swift rhythm of emergency responses to the slower, methodical pace of routine check-ups. Interoperability is the maestro, ensuring each section of this vast orchestra plays in tune, delivering a performance that's both efficient and error-free.
Navigating the Maze: Healthcare's regulatory landscape is an ever-evolving maze. But with interoperability as the guiding light, navigating becomes more manageable. It ensures compliance without compromise, safeguarding both patient trust and data integrity.
Competitive Advantage: According to Seib, as healthcare transitions to a value-based system from a fee-for-service model, the capacity to utilise data and transform it into valuable information will become a competitive advantage. By promoting interoperability with a modern standard like HL7® FHIR®, healthcare organisations can establish a foundation for prolonged success.
Regulations: The 21st Century Cures Act and the Information Blocking Rule by the US are all examples of how interoperability is front and centre in the new world order.
Interoperability isn't just a technical term; it's the lifeblood, ensuring every beat, every pulse, and every note aligns perfectly. In some cases, it may also decide your survival as a company.
Now it's time to give credit where it's due.
The Undisputed Champion of Healthcare Data Communication: HL7® v2.x
In their book Hacking Healthcare, the authors argue that
"Generally, standards that are more complex are more difficult to implement correctly across applications. As a result, simpler standards tend to become strong standards faster than complicated ones."
Trotter, Fred; David Uhlman. Hacking Healthcare.
They then go on to talk about how some protocols they consider "winning protocols".
"The protocols that get used in healthcare are not necessarily the best protocols for the job, but the protocols that "won" among implementors."
Trotter, Fred; David Uhlman. Hacking Healthcare.
And that is exactly what HL7® v2.x experienced back in the 80s and the 90s as an interoperability protocol.
It won.
Having been around since the late 1980s, HL7® v2.x enjoyed the first-mover advantage. This early introduction allowed it to set the tone for healthcare data communication, establishing itself as the de facto standard before alternatives even emerged.
First Mover Advantage: Being one of the earliest standards, HL7® v2.x had the opportunity to shape the industry's approach to data exchange. This early adoption meant that as newer healthcare IT systems were developed, they were often built with HL7® v2.x compatibility in mind. Over time, this created a self-reinforcing cycle: the more systems used HL7® v2.x, the more attractive it became for subsequent systems to adopt it.
The Cost of Change: Once a healthcare institution implemented HL7® v2.x and integrated it into its data pipeline, migrating to a different standard became both costly and disruptive. Transitioning requires financial investment, time, training, and potential workflow disruptions. This inertia often made sticking with HL7® v2.x a more appealing option, especially when it continued to meet the company's needs.
Economics and Ecosystem: Initial implementations of HL7® v2.x tended to be more cost-effective than newer standards. The abundance of tools, middleware solutions, and integration engines tailored for HL7® v2.x often meant that institutions can achieve their interoperability goals without hefty investments.'
Finally, given its long-standing history, a larger pool of IT professionals is familiar with HL7® v2.x. Hiring or training talent for a well-established standard is often easier and less expensive than newer, less widespread standards.
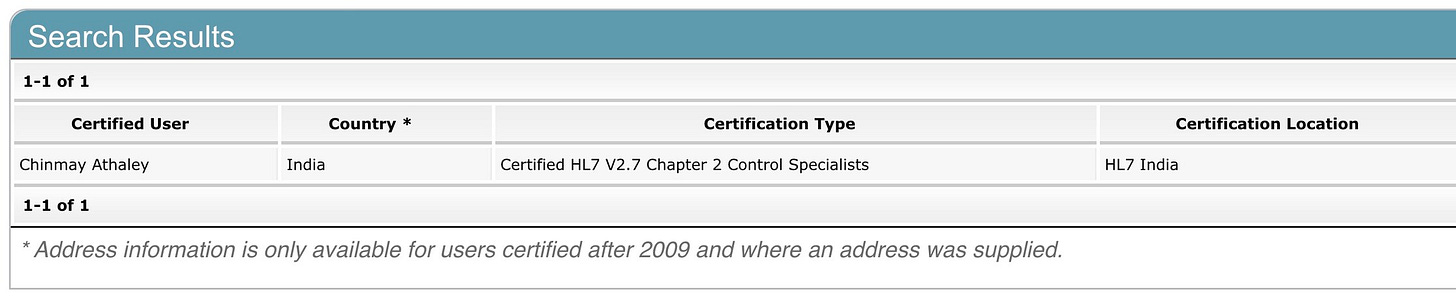
I went down the certification rabbit hole and scanned the HL7® certification directory to get the number of people certified across all certifications that HL7® has to offer. Here's the breakdown of this article as it was written.
This translates into the following % break up across the HL7® certification universe.
HL7® CDA certified members: 14.75%
HL7® v2.x certified members: 70.12%
HL7® v3 RIM certified members: 6.10%
HL7® FHIR® certified members: 9.06%.
Do you see the obvious?
As with many legacy systems, the very strengths of HL7® v2.x — its widespread adoption and the vast infrastructure built around it—also pose challenges. Transitioning away from such an entrenched standard is no small feat. It's not just about adopting a new standard; it's about ensuring it can communicate with the myriad systems still operating on HL7® v2.x.
HL7® website indicates that 95% of US healthcare organisations use HL7® v2.x compared to other HL7® standards.
While HL7® v2.x's dominance can be attributed to its technical merits, it's also a story of timing, economics, and the complexities of change in a sector as intricate as healthcare.
The HL7® Conundrum: Evolution Amidst Excellence
The journey of HL7® v2.x is akin to a seasoned athlete's career. While the athlete may have numerous accolades and records, they aren't immune to the wear and tear of time. Similarly, HL7® v2.x, despite its unparalleled dominance, isn't without its challenges.
Health Level Seven International is not just a custodian of standards; it's an entity driven by a mission. Founded in 1987, HL7®'s core objective has been to provide a comprehensive framework and related standards for exchanging, integrating, sharing, and retrieving electronic health information. Their vision? A world where everyone can securely access and use the correct health data when and where they need it. And this poses a very existential question(at least for HL7® v2.x). Should successful standards evolve? Why?
HL7® v2.x, for all its merits, was designed in a different era. As the healthcare landscape evolved, so did its requirements. The message-based standard sometimes struggles with modern healthcare systems' needs for real-time data exchange. Moreover, there is an increasing realisation that its lack of a standardised vocabulary can lead to ambiguities and challenging semantic interoperability. While HL7 v2.x does support the use of standardised vocabularies, it does not enforce it. This means that different implementations of HL7 v2.x might use different vocabularies for the same concepts, leading to potential ambiguities and challenges in achieving semantic interoperability. On the other hand, more modern standards like HL7® FHIR® are designed with semantic interoperability in mind and have more robust support for standardised vocabularies. This makes them better equipped to meet modern healthcare systems' real-time data exchange needs and ensure a consistent understanding of data across different systems.
Someone building a health tech organisation today is more likely to choose HL7® FHIR® over HL7® v2.x, given the ease of implementation in the modern tech world. The truth remains that introducing HL7® FHIR® doesn't diminish the legacy of HL7® v2.x. Instead, it probably highlights the need for harmonious coexistence. Many healthcare institutions find themselves in a delicate dance, honouring the established workflows built around v2.x while integrating the advancements offered by HL7® FHIR®. It's a testament to the resilience and adaptability of the healthcare IT community, ensuring that patient care remains at the forefront, irrespective of the standards in play.
So, where do we go from here?
Steering Through the HL7® Interoperability Standards Terrain
Navigating the world of healthcare interoperability is like charting a course through a dense forest. The tall and ancient trees represent established standards like HL7® v2.x, while the undergrowth and newer saplings symbolise emerging technologies and protocols.
HL7® v2.x has sheltered the healthcare community for decades with its deep roots and expansive canopy. It's essential to recognise its contributions and the stability it has provided. Just as seasoned travellers respect the landmarks that have guided them, healthcare professionals and institutions acknowledge the enduring relevance of v2.x.
The HL7® v2.x stands tall as the 800-pound gorilla in the vast jungle of healthcare interoperability. It is impossible to ignore, commanding respect and attention with its sheer presence. Just as a gorilla, with its strength and dominance, plays a pivotal role in maintaining the balance of its ecosystem, HL7® v2.x has been holding together the intricate web of healthcare data exchange. But the jungle is ever-evolving. New species emerge, each bringing its strengths and challenges. HL7® FHIR® is like the agile leopard, swift and adaptable, ready to climb the trees of modern technological advancements. Its agility contrasts with the gorilla's raw power, yet both are essential for the ecosystem's health. The challenge we face is not of dominance but of coexistence. How do we ensure that the 800-pound gorilla exists with the swift leopard? Should we leverage the strength and stability of HL7® v2.x while harnessing the flexibility and potential of HL7® FHIR®?
Or is it time for the old guard to step aside for the new?
As we venture deeper into this jungle, we must recognise the value each inhabitant brings. It's not about replacing the old with the new but about finding a harmonious rhythm where both can flourish. Can you completely replace 95% of your ecosystem that easily?
I think the future of healthcare interoperability is an act between the powerful gorilla and the agile leopard. And as we watch this act unfold, we are reminded that it's not just about standards or technologies. It's about creating a world where data moves gracefully, ensuring better care for all. Ultimately, the dance of interoperability is a testament to the power of collaboration and innovation, where every move and step is a stride towards a brighter, healthier future.
And lastly, for those of you still reading this and wondering what was the outcome of my HL7® v2.x certification exam attempt, I passed :).
References