The Anatomy of HealthTech
We have a company event coming up.
I was scouting for a performer, someone who could strike the right balance between English and Hindi music for a mixed audience.
I landed on an artist I had heard at a popular eating joint in Pune.
I messaged him about the requirements and discussed set duration, sound setup, and logistics.
Just as we were wrapping up, he casually dropped this …….
While I encourage the enthusiasm around HealthTech, I just wish everyone knocking on its doors understood that HealthTech is unlike any other tech.
Simply put, HealthTech exists to solve problems that arise out of the human body, the most sophisticated species on this planet! Reducing these problems to a health tech "MVP" would be an oversimplification.
Just as doctors study the anatomy of the human body, we HealthTech enthusiasts must make every effort to understand the anatomy of the system we are addressing.
Because technology is not the answer to all healthcare problems.
It never was.
What is non-negotiable, though, is that we understand the problems we are trying to solve.
And there is no better starting point for that than understanding the health system itself.
Understanding a ‘Health System’
The definition of a health system varies by context and geography. In the United States, it typically refers to networks of hospitals and healthcare providers focused on individual patient care. However, the World Health Organization (WHO) takes a broader view, defining a health system as all organisations, people, and actions aimed at improving the health of populations. This includes not just medical care but also public health initiatives, policies, and infrastructure.
We’ll go with the WHO definition for the purposes of this article.
A health system comprises multiple interconnected building blocks, each essential for delivering healthcare services. The World Health Organization (WHO) identifies six building blocks as the core.
Leadership and Governance: Includes setting strategic policies, building partnerships, regulating services, designing efficient systems, and ensuring accountability to maintain trust and integrity.
Health Workforce: Having enough trained healthcare professionals distributed fairly, responsive to patient needs, and working efficiently to provide the best possible care within available resources.
Health Information Systems: Collecting and analysing data on health trends, system performance, and population health status to inform policies and improve services.
Medical Products, Vaccines, and Technologies: Managing supply chains so that necessary medicines and tools reach those who need them.
Health Financing: Providing financial protection so individuals can access necessary care without suffering financial hardship and encourage efficient use of resources.
Service Delivery: This includes both personal medical care and broader public health interventions.
The list gives an impression that may be all the building blocks are equal. But in reality, they aren’t. Some elements form the foundation, while others depend on them to function.
So, I rank-ordered them based on what makes the most logical sense.
Leadership and Governance: Without leadership and governance, how do you decide where the money goes? How do you decide who regulates care? This is the foundation—it sets policies, regulations, and strategic direction.
Health Workforce: Policies and funding mean nothing without trained personnel. The workforce is the engine that drives care—without doctors, there would be no healthcare. Even if financing is limited, a strong workforce can deliver care.
Health Financing: Financing supports everything else—but it's not the starting point. Good policies and a trained workforce make financing more effective.
Medical Products, Vaccines, and Technologies: Even if you have money, you need governance and a workforce first to distribute medical products effectively. Supply chains depend on regulations, trained personnel, and funding.
Service Delivery: This is the ultimate goal, but it only functions well if leadership, workforce, financing, and supplies are aligned. Bad governance = Inefficient service delivery (e.g., underfunded public hospitals, overburdened doctors). Service delivery is where all other components come together.
Health Information Systems: This is a feedback loop, not a foundational pillar. Data helps optimise, refine, and improve efficiency, but it doesn’t treat patients, distribute funds, or train doctors. AI-powered diagnostics are useless in hospitals without doctors, funding, and medical supplies.
Healthcare technology is most effective when built upon a well-governed system, supported by capable professionals, essential resources, and sustainable funding—all culminating in high-quality service delivery, which is then refined and improved through robust health information systems.
While much can be written on the first 5 building blocks, I am here to discuss #6 today.
WHO calls it ‘Health Information Systems,’ but that feels outdated. Today, that system is much broader. It doesn’t just collect and analyse data but actively transforms healthcare delivery. From AI-driven diagnostics to real-time disease surveillance, technology is more than just an ‘information system’. So, I will take the liberty of renaming the last building block to ‘Health Technology’ so we can double-click on it.
We could argue that ‘Health Technology’ can be broadly divided into 2 categories.
Public Health Technology: This encompasses systems and innovations that address population-wide issues (e.g., disease surveillance, environmental monitoring, and water and air quality management). These technologies support public health initiatives and policy frameworks aimed at preventing disease and promoting well-being on a large scale.
Healthcare Technology: This category focuses on clinical settings and institutional care. It includes the tools and systems that support the delivery of medical services—like electronic health records, telemedicine platforms, diagnostic equipment, and hospital management systems—which directly influence patient outcomes in healthcare facilities.
This brings us to a critical question.
What exactly is healthcare? And how is it different from public health?
Healthcare Vs Public Health
We use the words ‘healthcare’ and ‘public health’ interchangeably. But they are not the same. In fact, the difference between the two is fundamental to defining the role that technology can potentially play in each of these domains.
Healthcare is about individual treatment and care. Hospitals, doctors, medicines, surgeries, diagnostics. It focuses on curing or managing diseases at a personal level.
Public Health, on the contrary, is about populations. Vaccination programs, sanitation, disease prevention, and policy interventions. It aims to prevent diseases and promote health at scale.
While both use technology to improve health outcomes, their application is different.
Now, think about this.
Who funds tech in each of these domains?
Most HealthTech investments focus on individual healthcare because they are profit-driven. Private players invest in hospital-based tech, diagnostics, and drugs because these offer financial returns.
Public Health Tech, however, often requires state backing because it lacks an immediate revenue model or “exit” option.
Public health investments take years or decades to show results. Neglecting public health creates avoidable disease burdens that HealthTech alone cannot solve. And this, my friends, is the endless loop we are stuck in.
Let us talk about how nations allocate their health budgets.
In high-income countries, public health receives less than 10% of the total health budget (e.g., US: ~5%, Germany: ~8%). Most spending goes toward hospitals, specialists, and pharmaceuticals rather than disease prevention. Low-income countries tend to underfund both healthcare and public health. Countries with more substantial public health investments see better long-term outcomes. For example, Nordic countries (Sweden, Denmark, Norway) spend about 10% of their GDP on Health. Germany has a unique distinction in terms of having the highest health expenditure in the EU.
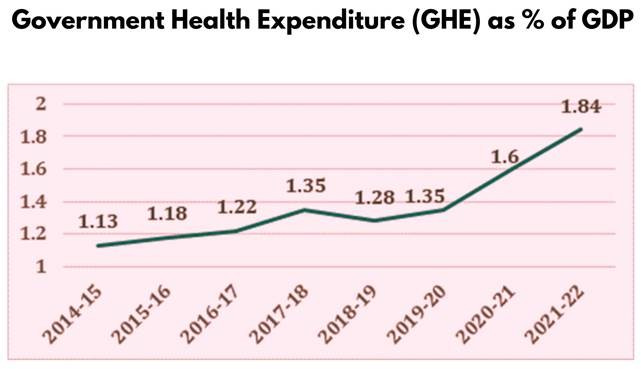
India spends just ~1.9% of GDP on health, and most still goes toward curative care. Remember, Ayushman Bharat (PMJAY) is primarily a hospital-based insurance program, not a public health initiative.
The U.S. spends the most on healthcare (~17% of GDP). But here’s the shocking part—90% of the nation’s $4.5 trillion spending goes to managing chronic and mental health conditions.
India's case is different. India must prioritise public health first. Clean water, sanitation, vaccines, and nutrition deliver higher returns than simply expanding hospitals and insurance coverage.
Preventive health investments (e.g., vaccination, nutrition, and sanitation) can reduce the disease burden, decrease overall costs, and improve long-term economic productivity. Below is the % allocation of India’s health expenditure, taken straight from the official government website.
Don’t get me wrong. I loveeee PMJAY. However, PMJAY is primarily a publicly funded health insurance scheme that provides financial protection for secondary and tertiary hospitalisation to economically vulnerable families. While it enhances access to healthcare services, it focuses on curative care rather than public health initiatives like disease prevention, health education, and sanitation.
But something feels counterintuitive. Nations could potentially allocate a significant health budget to public health, but that does not happen. The theme, which remains the same across developed and developing countries, is that spending is still focused on
How much of your nation’s GDP should go to healthcare?
How do you divide that budget between public health and healthcare services?
What other critical areas need investment?
This is a fabulous rabbit hole to go down, but not in this article.
Private Sector - higher insurance claims, lower productivity.
Society - a rising disease burden, a weaker workforce.
Future Governments - higher long-term healthcare costs.
Citizens - higher out-of-pocket expenses and a poorer quality of life.
Sounds like doomsday, doesn’t it?
Can we be rescued at all?
Enter HealthTech
You might wonder, why are we discussing technology only now in an article that was supposed to be discussing its ‘anatomy’? Shouldn’t it have been the first topic?
Like any other technology, healthtech is not the starting point. It can be a response and an enabler, but not the foundation.
Abraham Maslow said, "To a man with a hammer, everything looks like a nail." I’m afraid the tech community increasingly views healthtech as a panacea. But nothing can be farther from the truth. We must first understand it. And to understand what healthcare technology is, we should first understand what it is not.
HealthTech is not a substitute for a fully functioning health system.
Healthcare is not a substitute for public health interventions.
HealthTech is not a solution for poor policy and governance.
HealthTech is not a replacement for doctors and human judgment.
Healthcare is not a magic bullet that will fix healthcare costs.
But what is HealthTech, then? Does it have a definition? Well, it does - many. Of all the definitions, I like the one from HIMSS the most.
“Healthcare Technology empowers people and populations to manage health and wellness, augmented by accessible and supportive provider teams working within flexible, integrated, interoperable and digitally-enabled care environments that strategically leverage digital tools, technologies and services to transform care delivery.” This definition captures the full scope of Healthcare Technology, but I feel it’s still abstract. What does it actually mean in practice?
To answer this question, let's extract the key phrases from the definition itself and use them as a framework to understand the broad HealthTech categories.
"Empowers People and Populations to Manage Health and Wellness" = Consumer HealthTech & Remote Care
This is one of the most visible transformations in modern healthcare. From wearables that track heart rates to AI chatbots that provide mental health support, these devices give people greater control over their well-being, enabling them to take proactive steps before medical intervention is needed. One of the best examples of this shift is Continuous Glucose Monitors (CGMs) like Freestyle Libre.
Traditionally, diabetics had to prick their fingers multiple times a day to check blood sugar levels. Now, CGMs automatically track glucose levels in real-time, sending alerts to smartphones when intervention is needed. This directly results in fewer hospital visits, better disease management, and higher quality of life. And CGMs are just one part of this revolution.
Consumer HealthTech spans a range of powerful tools that are reshaping how we engage with our own health
Wearable Devices & Remote Monitoring – Smartwatches like Apple Watch & Fitbit detect irregular heart rhythms, while CGMs help diabetics manage glucose levels.
Mobile Health(mHealth) Apps – AI-powered mental health apps like Wysa provide on-demand therapy, while telemedicine platforms like Practo connect patients to doctors remotely.
Personalised Digital Therapeutics (DTx) – Prescription digital therapies use AI-driven interventions for mental health, addiction, and chronic disease management.
“Augmented by Accessible and Supportive Provider Teams” = Tech for Healthcare Providers
This is where HealthTech works with doctors, nurses, and medical staff to enhance decision-making and improve patient outcomes. Healthcare professionals don’t see technology as a replacement but as a highly capable assistant that helps them work more efficiently, reduce errors, and expand access to care.
One of the best examples is Qure.ai, an AI-powered radiology tool used in India. Many rural hospitals lack trained radiologists, which delays diagnoses for diseases like tuberculosis and pneumonia - a leading cause of preventable deaths in lower-income settings. Qure.ai’s system analyses X-rays in seconds, flagging abnormalities so doctors can intervene faster. This helps triage efficiently and route only those cases that actually need attention from a doctor, thereby helping solve access.
This is a classic example of how AI doesn’t replace doctors - it augments them, making expert-level care more accessible in resource-limited settings.
And this is just one of the ways technology can assist healthcare providers. Across hospitals, clinics, and telemedicine platforms, HealthTech is supercharging medical professionals through a variety of tools:
Clinical Decision Support Systems (CDSS) – AI-driven tools like Qure.ai help doctors identify diseases faster and reduce misdiagnoses.
Telemedicine & Virtual Care Platforms – Platforms like eSanjeevani, Teladoc, and Amwell enable remote consultations, ensuring that even patients in remote areas get expert medical advice.
AI & Automation in Hospitals – AI-assisted robotic surgery and hospital automation optimize workflows, allowing faster diagnoses, better triage, and smoother hospital operations.
“Flexible, Integrated, Interoperable and Digitally-Enabled Care Environments” = Health Information Systems & Standards.
This is where technology ensures that patient data moves as seamlessly as the patients themselves. Your medical records shouldn’t be trapped in one hospital or doctor’s office, right? Imagine switching hospitals and having to redo all your tests just because your medical history doesn’t transfer. That’s what happens when health data is fragmented. It leads to delays, unnecessary costs, and poor care coordination.
This is exactly what India’s Ayushman Bharat Digital Mission (ABDM) is trying to solve.
By creating a unified digital health ID, ABDM allows patients, hospitals, and insurers to securely access medical records nationwide, reducing redundant tests, preventing administrative bottlenecks, and ensuring continuity of care. The key to making this work is interoperability standards like HL7 FHIR, SNOMED, DICOM, etc., enabling seamless health data exchange across different systems. I have written a short LinkedIn post about the various health tech standards available at our disposal if you want to know more about this. I have also differentiated standards from formats in another LinkedIn post.
Think of these interoperability standards as the backbone of modern Health Technology. Without standardised health data, technology becomes isolated islands of information rather than a connected healthcare ecosystem. ABDM is just one part of a larger movement towards seamless, secure, and standardised healthcare information.
Some of the critical technologies driving this shift include:
Electronic Health Records (EHRs) - Platforms like Epic and Cerner ensure that doctors have real-time access to patient history, improving clinical decisions.
Interoperability & Health Data Standards – Protocols like HL7 FHIR, DICOM, and SNOMED-CT enable different health systems to speak the same language, reducing data silos.
Health Information Exchanges (HIEs) & Data Privacy Regulations – HIPAA (U.S.), GDPR (Europe), and ABDM’s Health ID (India) protect patient data while allowing secure, consent-based data sharing.
"Strategically Leverage Digital Tools, Technologies, and Services to Transform Care Delivery" = AI & Emerging Technologies in Healthcare.
This is where HealthTech moves beyond digitisation and into the realm of discovery, prediction, and automation. Healthcare is no longer just about records and wearables—we are now at the frontier of transforming medicine itself. AI detects diseases before symptoms appear, blockchain secures medical data and drug supply chains, and predictive analytics helps governments preempt pandemics.
One of the most groundbreaking examples of this is DeepMind’s AlphaFold.
Drug discovery has always been painfully slow. Scientists need to experimentally determine how proteins fold into 3D structures, a process that can take years if not decades. Protein folding is key to understanding diseases like cancer, Alzheimer’s, and antibiotic resistance, but the complexity of this biological puzzle makes progress frustratingly slow.
Then came AlphaFold on the scene.
Using deep learning algorithms, AlphaFold predicted the structures of 200 million proteins in days, solving a 50-year-old scientific problem and revolutionising drug development. The impact? New treatments for life-threatening diseases can now be developed faster, cheaper, and more precisely than ever before. This is the edge of HealthTech. Not just digitising healthcare but redefining how we understand and treat diseases. And AlphaFold is just one part of a larger movement where AI and emerging technologies are radically transforming care delivery:
Artificial Intelligence in Diagnostics & Drug Discovery – AI tools like DeepMind’s AlphaFold and IBM Watson are accelerating medical research and improving early disease detection.
Big Data & Predictive Analytics in Public Health – AI-driven epidemic forecasting helps governments predict disease outbreaks before they spread, enabling faster interventions.
Blockchain for Healthcare Security & Supply Chain – Decentralized systems protect patient records from cyberattacks and track drug authenticity to prevent counterfeit medicine.
But here’s the reality - technology alone isn’t enough.
AI can detect diseases early, blockchain can secure health data, and predictive analytics can help governments prevent pandemics. But without the right policies in place, even the most groundbreaking health technologies struggle to scale, remain inaccessible, or worse, cause more harm than good.
Take the U.S. HITECH Act, for example. The widespread adoption of Electronic Health Records (EHRs) was primarily a policy intervention. Similarly, India’s Ayushman Bharat Digital Mission (ABDM) was a policy-driven attempt to create an interoperable, consent-based health data exchange.
HealthTech doesn’t exist in a vacuum. It evolves within legal, ethical, and economic frameworks. Whether the HITECH Act drives EHR adoption, the GDPR shapes data privacy in Europe, or ABDM enables digital health interoperability in India, policy decisions determine how, where, and for whom healthcare technology works.
The Role of Policy in HealthTech
Before we explore how policy shapes Health Tech, we need to step back and ask: What does policy actually do? Why does it exist, and how does it guide decision-making in complex sectors like healthcare and technology?
And here, I will rely on the notes from my policy class at The Takshashila Institution from way back in 2020!
One of the best ways to understand how policymakers approach complex problems is through Eugene Bardach’s Eightfold Path, a widely used framework for policy analysis and decision-making. It offers a structured way to evaluate policy choices, government intervention, and resource allocation, especially in sectors like healthcare and technology, where trade-offs are inevitable.
So, let’s apply Bardach’s framework to HealthTech policy.
Define the Problem: What issue needs to be addressed? (e.g., lack of EHR interoperability, Data privacy, Tech adoption).
Assemble the Evidence: What data supports the need for intervention? (e.g., studies showing fragmented health records lead to misdiagnoses).
Construct the Alternatives: What are the possible policy options? (e.g., government-mandated EHR standards vs. voluntary adoption).
Select the Criteria: What makes a policy solution viable? (e.g., cost-effectiveness, equity, scalability, access).
Project the Outcomes: What are the potential impacts of each alternative?
Confront the Tradeoffs: What are the downsides of each policy choice? (e.g., privacy concerns vs. efficiency gains in ABDM).
Decide: Choose the best course of action based on analysis.
Tell Your Story: Communicate why the policy is needed and how it will be implemented.
Policymakers don’t just regulate technology for the sake of regulation. They apply structured decision-making models like Bardach’s to weigh trade-offs before implementing policies. This is especially true for countries like India, which have low state capacity.
But policy-making lies with the government. I am a big fan of the book ‘In Service of The Republic’ by Ajay Shah and Vijay Kelkar. One key theme I picked up from that book is that laissez-faire should be the de facto mode of any government. And the question then becomes: When should the government intervene?
Governments should intervene in free markets when there is:
Market Failure: When private companies alone can’t provide essential services.
Example: Rural healthcare infrastructure is often unprofitable for private providers, and hence, it makes sense for governments to invest in telemedicine initiatives like eSanjeevani in India to fill the gap.
Public Goods & Externalities: When investment benefits extend beyond individual users.
Example: Vaccination programs: Private markets may not invest enough, so governments should subsidise or mandate them to protect public health.
Equity & Access Issues: When market-driven solutions create disparities.
Example: AI-based diagnostics may be expensive and benefit only wealthier patients and hence governments should create incentives for universal adoption (like HITECH’s EHR incentives).
Regulation of Safety & Privacy: When unregulated innovation poses risks.
Example: AI-driven clinical decisions could lead to misdiagnoses and hence governments should enforce accountability and liability frameworks to ensure patient safety.
Blinkit, a popular quick commerce platform from India, was bored with doing 10-minute grocery deliveries. So, they pushed the envelope by starting a 10-minute Ambulance service! But this is a classic case of a free market highlighting a deeper problem in a healthcare system.
In the editorial, the author argues that there is a need for standardisation of ambulance services in India.
This needs government intervention and, thereby, policy!
Policy serves three critical roles in shaping HealthTech:*
Regulation & Standardization: Setting technical and ethical standards that ensure safety, privacy, and interoperability.
Incentivization & Adoption Acceleration: Driving faster adoption of beneficial technologies through funding, incentives, and mandates.
Bridging the Public-Private Gap: Ensuring underserved populations have access to HealthTech, preventing innovation from being exclusive to the wealthy."*
Policy isn’t just about regulation. It’s about shaping how technology is adopted, scaled, and safeguarded.
HITECH Act (U.S.) drove mass EHR adoption by offering financial incentives to hospitals, digitizing patient records nationwide. However, poor system design led to physician burnout, highlighting the importance of usability in policy-driven tech adoption.
ABDM (India) established a nationwide digital health infrastructure, enabling secure, consent-based data exchange via a unified health ID. Its success hinges on hospital participation, interoperability, and strong data privacy enforcement.
GDPR (Europe) defined global standards for health data privacy, enforcing strict patient consent and security laws. While it strengthened patient rights, compliance burdens increased for HealthTech companies, slowing innovation in some cases.
These policies highlight a fundamental truth: Technology doesn’t drive change independently, policy defines its impact. It shapes who benefits, how widely innovations scale, and what risks are managed or overlooked.
So far, we’ve dissected Health Technology piece by piece, from its foundations and applications to the policies that govern it. Like studying the anatomy of the human body, understanding Health Technology requires knowing how its systems interact, where its vulnerabilities lie, and how external forces (like policy) dictate its function.
But there’s one force that isn’t just influencing HealthTech. It’s rewriting its very blueprint.
A force so powerful, so unpredictable, that it demands an entirely new way of thinking.
The Black Swan
Artificial Intelligence has been around for decades. We’ve seen it in rule-based systems, machine learning models, and automation tools, chipping away at inefficiencies but never quite shaking the world.
Then came 2022.
ChatGPT casually dropped GPT 3.5.
And just like that, everything changed.
AI was no longer just a tool for data scientists or backend engineers; it was on everyone’s screen, in everyone’s conversations, and in every industry. This train had left the station, and it wasn’t showing any signs of slowing down. Fast-forward a few years, and we’re no longer talking about the ‘what’ of AI; the conversation has changed to the ‘how’ of AI. This AI wave isn’t just transformative; it’s disruptive.
And there’s one industry that desperately needs disruption…….
The Global AI Index developed by Tortoise Media closely examines artificial intelligence development in 83 countries, assessing their AI capabilities based on 122 distinct indicators. These indicators fall into three core categories: Implementation, Innovation, and Investment.
We are spending 10.4% of the global GDP on healthcare. That’s $9.8 trillion every year. At the same time, we have this almost magical AI superpower handed over to us. This is serendipity. But serendipity is fleeting. We need to act on it before the moment slips away.
The question is: How do we use Artificial Intelligence in healthcare?
We can approach this from a couple of different angles.
Administrative Overhead: Administrative costs account for approximately 34% of healthcare spending in the United States, which, according to a study, was $812 billion in 2017. AI assistants like Nuance DAX help doctors dictate patient notes in real time, reducing electronic health record (EHR) fatigue.
Hospital Operations: Hospitals incur substantial losses annually due to inefficient resource allocation, avoidable readmissions, and bed shortages. Predictive AI can forecast ICU demand, optimise surgery schedules, and automate discharge planning, reducing bottlenecks. Johns Hopkins spun up a Capacity Command Center, which used AI to enhance patient flow and operational efficiency. This led to a 70% reduction in transfer delays from operating rooms, a 30% faster assignment of beds for emergency room patients, and a 60% improvement in accepting complex medical cases from other hospitals.
Early Diagnosis and Disease Prevention: Researchers from Google Health and DeepMind created an AI system to identify breast cancer in mammogram images more accurately than human doctors. This AI made fewer mistakes when diagnosing cancer, showing a 9.4% decrease in missed cases (false negatives) and a 5.7% reduction in incorrect diagnoses (false positives) in data from the United States. In the UK, it also showed improvements, with 2.7% fewer missed cases and 1.2% fewer incorrect diagnoses.
Drug Discovery: Developing a new drug is both time-consuming and expensive. A Deloitte report indicates that bringing a new drug to market costs approximately $2.3 billion and takes over a decade. AI can analyse molecular structures, predict drug interactions, and simulate clinical trials, thus reducing both time and costs in drug development. DeepMind’s AlphaFold has made significant advancements in predicting protein folding, which accelerates drug discovery for diseases such as Parkinson’s.
Public Health and Epidemiology: According to a Harvard Study, the global economy suffered a loss of $16 Trillion due to the COVID-19 pandemic. BlueDot, a Canadian health monitoring startup, utilised its AI-driven platform to analyse vast amounts of data, including foreign news reports and airline information, to identify the emerging threat of COVID-19. The platform alerted its clients on December 31, 2019, regarding the novel coronavirus outbreak, days before major public health authorities, including the WHO, made official statements.
There are many other ways AI could reshape healthcare, each a potential attempt at solving the $9.8 trillion problem.
Will it lower costs? Probably.
Will it increase access? Almost certainly.
Will it change lives? Without a doubt.
And this, my fellow HealthTech enthusiasts, is the anatomy of HealthTech.
It’s not just about having the technology. It’s about applying it to the problems that matter.
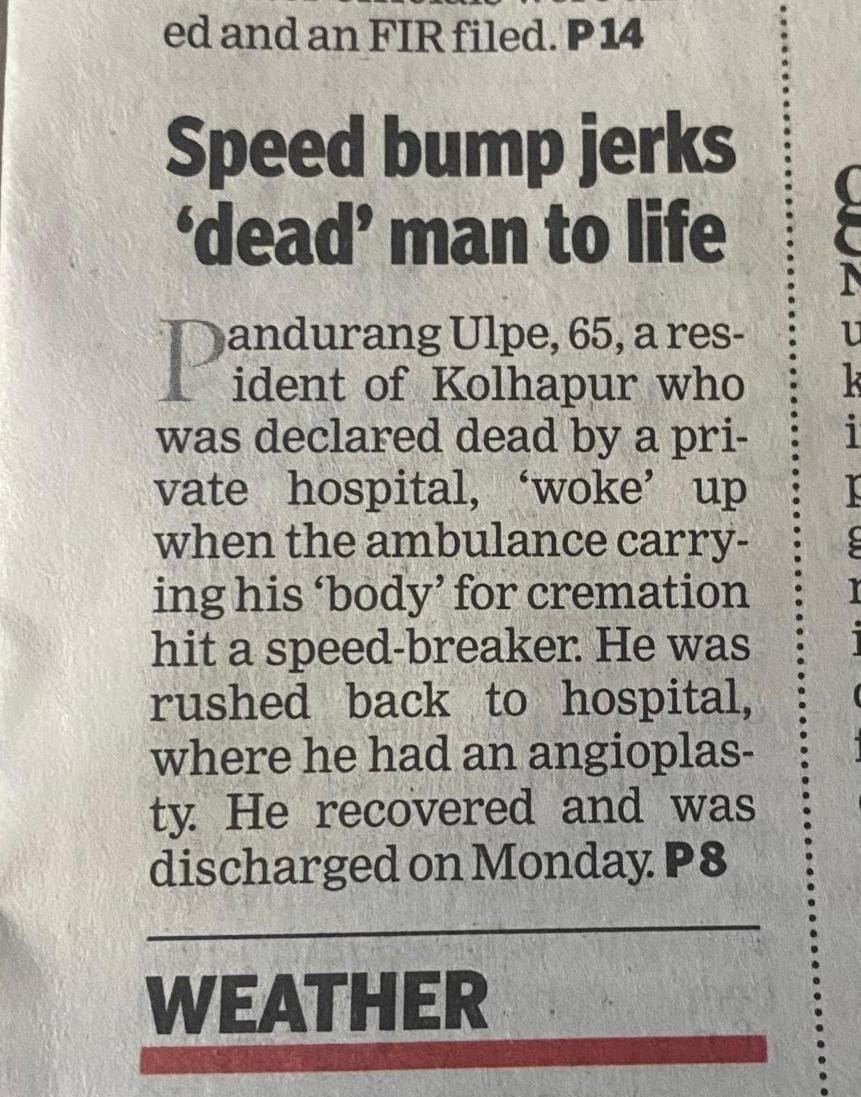
On a lighter note, for all the artificial intelligence, automation, and digital breakthroughs we have at our disposal, nothing beats the ability to bring people back from the dead.
You can’t make this up.
This is a REAL STORY.
References
India: PMJAY dashboard