From Ayurveda to Artificial Intelligence: A Brief History of India’s Healthcare Evolution
On April 21, 2023, India surpassed China to become the world’s most populous nation. Known as the land of diversity, India was always known for its rich cultural heritage and age-old medical practices. Today, with a population that big, healthcare has become a topic more important than any other in India. As the country modernises, the demand for quality healthcare has grown exponentially. From ancient Ayurvedic remedies to cutting-edge AI-driven healthcare solutions, the evolution of healthcare in India is a story of innovation, adaptation, and transformation.
A Glimpse of Healthcare in Ancient India
India’s evidence of medical knowledge and healthcare practices dates back to the Indus Valley Civilization, which flourished between 2600 BCE and 1900 BCE. The ancient Indian system of medicine, Ayurveda, is believed to have originated during this time and has been practised for over 5,000 years. Ayurveda operates on the philosophy of striking a balance between the body, mind, and spirit and using natural herbs and minerals to cure diseases. The knowledge of Ayurveda was passed down orally across generations until it was compiled into written texts, such as the Charaka Samhita and the Sushruta Samhita, in the 6th century BCE. But this was not the first ancient text of India that was “written.” That is believed to be Rigveda.
It is in Rigveda and Atharvaveda that the concept of ‘healing’ actually exists in the form of hymns. And here is where things get divine. It is believed that the Vedas were revealed only to sages known as "Rishis" through meditation and spiritual experiences. The Rishis then passed on this knowledge through an oral tradition to their disciples, who continued the tradition of memorising and reciting the Vedas. These texts were written sometime between 1700 BCE and 1000 BCE. The dates of these texts are still debated among scholars, and there is no consensus on the exact timeline of their composition. But we can safely say that even if we are off by a century, we are still talking about something written over 40 centuries back. In a world where things get forgotten within days, the very survival of these texts over several millennia means something. So, what was it in the Rigveda really that inspired a discipline as big as Ayurveda?
A shloka in Book 10, Hymn 97.
Rigveda 10.9
अथर्वणस्तथा वेदो यजूंषि सामानि च।
जगतः सर्वमायुर्विश्वामित्रं च भेषजम्॥
यदस्मिन्नद्भुतं रोगं व्यश्ञयन्ति दक्षिणाः।
उप ते सहस्रं विश्वमायुरस्तु देहि मे॥A rough English translation of the shloka is as follows.
The Atharvaveda, the Rigveda, the Yajurveda, and the Samaved
Comprise the life-span of the universe and the remedy for all disorders
Whatever ailments are in this body
May a thousand types of remedy bestow on me the highest life-spanAs you can tell, the shloka above does not necessarily refer to medicine as a specific practice or field of study but does mention the concept of healing and diseases. There are several such hymns. These hymns focused more on seeking help from the divine for healing and protection from diseases. These hymns are considered the foundation of Ayurveda, the ancient Indian system of medicine.
So, how did Ayurveda draw upon these ancient texts?
Several sources mention that the practice of Ayurveda is based upon the core idea, found in the Atharvaveda and Rigveda, of the healing power of nature and the emphasis on maintaining a balance between the body, mind, and spirit. Ayurveda drew upon these ideas to develop a holistic approach to medicine, focusing on the individual rather than just treating specific symptoms or diseases. In particular, Ayurveda borrowed from the Rigveda and Atharvaveda the idea of three doshas or humors: vata, pitta, and kapha. These doshas represent different aspects of bodily function and are believed to influence a person's physical, mental, and emotional characteristics. Ayurvedic practitioners aim to promote health and prevent disease by understanding and balancing these doshas. Ayurveda also drew upon the use of herbs and plants for medicinal purposes, which was a common practice in ancient India. The Rigveda and Atharvaveda contain numerous references to medicinal plants and their healing properties, which served as the basis for Ayurvedic pharmacology. The principles and practices of Ayurveda have their roots in the wisdom and knowledge contained in the ancient texts of Rigveda and Atharvaveda. Several texts are considered foundational to Ayurveda and are still widely studied and referenced in modern Ayurvedic practice.
Some of the most important texts include:
Charaka Samhita: This text, attributed to the sage Charaka, is one of the oldest and most influential Ayurvedic texts. It covers various topics, including anatomy, physiology, diagnosis, and treatment, and is still used as a reference by Ayurvedic practitioners today.
Sushruta Samhita: This text, attributed to the sage Sushruta, is another important Ayurvedic text that deals primarily with surgical procedures. It is notable for its detailed descriptions of surgical instruments and techniques, many of which are still used in modern surgery.
Ashtanga Hridaya: This text, written by the physician Vagbhata, is a concise and practical guide to Ayurvedic medicine. It covers topics ranging from diagnosis and treatment to diet and lifestyle recommendations.
Bhava Prakasha: This text, written by the physician Bhavamisra, is a comprehensive guide to Ayurvedic pharmacology. It includes detailed descriptions of hundreds of medicinal plants and their uses in Ayurvedic medicine.
These texts are still studied and revered by practitioners of Ayurveda and are considered essential for anyone seeking to understand the principles and practices of this ancient system of medicine. Having said that, Ayurveda faces criticism from some quarters primarily for the following reasons.
Lack of scientific evidence: Some medical practitioners criticise Ayurveda for lacking scientific evidence to support its claims and efficacy. Ayurvedic treatments and medicines are often not tested through randomised controlled trials, the gold standard for testing medical interventions.
Safety concerns: There have been cases where Ayurvedic medicines were found to be contaminated with heavy metals or other toxic substances, which can be harmful. Some Ayurvedic practitioners also use unsterilised instruments or administer treatments in unsanitary conditions, which can lead to infections.
Lack of standardisation: Ayurvedic treatments and medicines are often not standardised in dosage, quality, or purity. This lack of standardisation can lead to variations in efficacy and safety across different practitioners and products.
But while there may be critics, the fact remains that Ayurveda has managed to capture the imagination of millions (billions now?) of Indians for centuries. It is deeply ingrained in the Indian culture, with many relying on Ayurvedic remedies and treatments for their health and well-being. The Indian government has also been promoting Ayurveda as a part of its healthcare initiatives, formalising a Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homoeopathy (AYUSH), formed in 2014 to promote Ayurvedic and alternative medicine in India. Ayurveda remains an integral part of India's cultural and medical heritage and continues to play a significant role in the country's healthcare landscape.
However, the arrival of Western colonial powers in the 18th and 19th centuries brought in a challenger brand that would significantly change the healthcare landscape in India.
Enter modern medicine.
The emergence of modern medicine in India
With the British East India Company's colonisation of India, western medical knowledge and practices were introduced to the country, eventually leading to the establishment of modern medical institutions. The first modern medical college in India was established in Kolkata in 1835, followed by medical colleges in Bombay (1845) and Madras (1850). These institutions followed the Western model of medical education and focused on modern medical knowledge and practices. Modern medicine soon gained popularity, especially among the elite classes and in urban areas, and was seen as a symbol of modernity and progress. There were significant Indian figures who contributed to the growth and evolution of modern medicine in India. One of them was Dr Bidhan Chandra Roy.
Dr Bidhan Chandra Roy was a prominent physician and freedom fighter who played a significant role in the development of modern medicine in India. He is known for his contribution to the establishment of the Indian Medical Association (1928), which is now the largest association of medical professionals in India. He founded the Medical College and Hospital in Kolkata, one of the country’s premier medical institutions. Dr Roy became the Chief Minister of West Bengal from 1948 until he died in 1962. During that time, he played a vital role in developing healthcare infrastructure in the state.
Sir M. Visvesvaraya was another such figure. A prominent engineer, statesman, and reformer who significantly contributed to modern medicine’s development in India. Sir Visvesvaraya was a strong advocate for public health and sanitation. He served as the Dewan of Mysore State, where he introduced several measures to improve public health, including establishing hospitals, clinics, and sanitation facilities.
In the 20th century, modern medicine continued to grow and expand in India. The Indian Medical Association played an essential role in developing and regulating modern medicine in the country. Modern medical institutions, such as the All India Institute of Medical Sciences (AIIMS) and the Post Graduate Institute of Medical Education and Research (PGIMER), were established to provide high-quality medical education and healthcare. The contribution of these individuals, coupled with the establishment of institutions like the Indian Medical Association, laid the foundation for the rapid development and regulation of modern medicine throughout the 20th century in India. Their vision and efforts propelled the expansion of medical education, establishing specialised hospitals, and advancing research and innovation. These pioneers focused on improving medical infrastructure and prioritised healthcare practitioners' training and professional development. This comprehensive approach facilitated the growth of modern medicine across various medical disciplines, including surgery, internal medicine, paediatrics, and gynaecology.
Despite the advancements in modern medicine, India has upheld its rich traditional healing practices, such as Ayurveda, Yoga, and Naturopathy. Integrating these ancient systems with modern medicine has been an ongoing discussion and pursuit. Recognising the value of holistic approaches to healthcare, efforts have been made to promote an integrative approach that combines the strengths of both modern medicine and traditional healing practices. This evolving paradigm seeks to provide comprehensive and patient-centred care, embracing India's diverse healthcare traditions while ensuring evidence-based and scientifically validated treatments.
As we look to the future, the convergence of modern medicine, traditional healing practices, and innovative healthcare approaches hold immense potential for addressing the healthcare challenges of a diverse and complex society. This collective pursuit aims to achieve the highest healthcare standards, improve health outcomes, and ensure equitable access to quality medical services for all individuals across India.
Post-independence healthcare in India
One cannot talk about the post-independence healthcare initiatives in India without discussing a seminal event that occurred pre-independence.
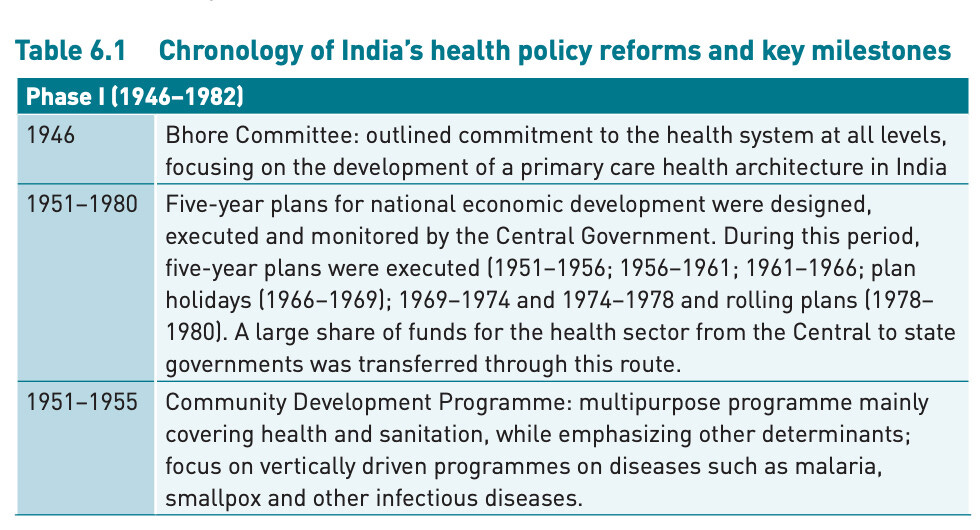
That event was the commissioning of the Bhore Committee Report.
The Bhore Committee Report was commissioned in 1943 by the British colonial government, grappling with a shortage of healthcare infrastructure and staff in the country. The committee was led by Sir Joseph Bhore, a British physician tasked with making recommendations for developing a comprehensive healthcare system for India. At the time, India was still a colony of the British Empire, and the healthcare system was primarily geared towards meeting the needs of the colonial rulers rather than the Indian population. Most Indians had little access to modern medical care, and traditional medical systems such as Ayurveda, Unani, and Siddha were not integrated into the mainstream healthcare system. Therefore, the Bhore Committee Report was a seminal document that laid out a blueprint for developing India's modern and comprehensive healthcare system. The report emphasised the need for preventive healthcare measures like sanitation and hygiene and training and recruiting more healthcare personnel, including doctors, nurses, and midwives. The report also discussed integrating traditional Indian medical systems into mainstream healthcare. It recommended the establishment of medical colleges and research institutions to promote the study and development of these systems.
The recommendations of the Bhore Committee report laid the foundation for India's modern healthcare system and significantly shaped the country's healthcare policies and programs. The primary recommendations were as follows.
Creation of a national health service that would provide free and comprehensive healthcare to all citizens of India.
The number of healthcare facilities, including hospitals and dispensaries, be increased to ensure that everyone has access to healthcare.
Increasing the number of healthcare workers, including doctors, nurses, and midwives, to meet the growing demand for healthcare services.\
Healthcare infrastructure be improved, including constructing new hospitals, upgrading existing facilities, and establishing healthcare research centres.
Creating a system to train and educate healthcare professionals, including doctors, nurses, and midwives.
Establishment of disease control measures, including vaccination programs, to prevent the spread of diseases.
Establish a robust public health administration responsible for nationwide planning, implementing, and monitoring healthcare programs.
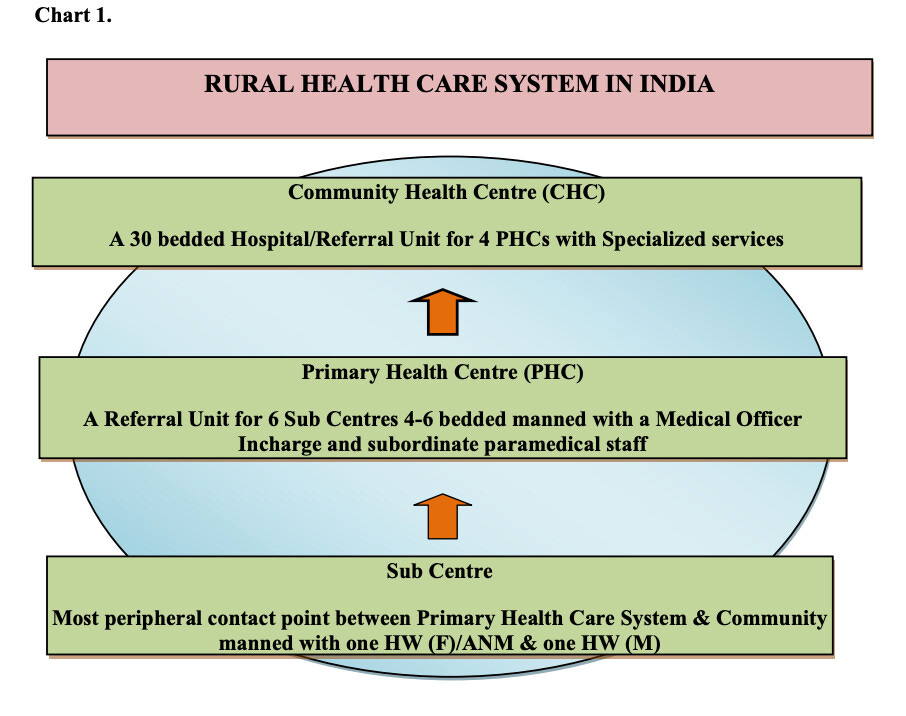
The Bhore Committee report emphasised establishing primary health centres (PHCs) throughout the country, which is very visible even today. The report recommended the establishment of one PHC per 10,000 people in rural areas and one for every 30,000 people in urban areas. This led to the establishment of thousands of PHCs in the country, which provided primary healthcare services to millions of people who previously had little or no access to healthcare. But India is diverse. The definition of what is “rural” even is debatable. India saw the need to take the idea of PHCs further and develop it into a three-tier healthcare infrastructure for rural India. Community Health Centers (CHCs) and Sub Centres were born from this idea.
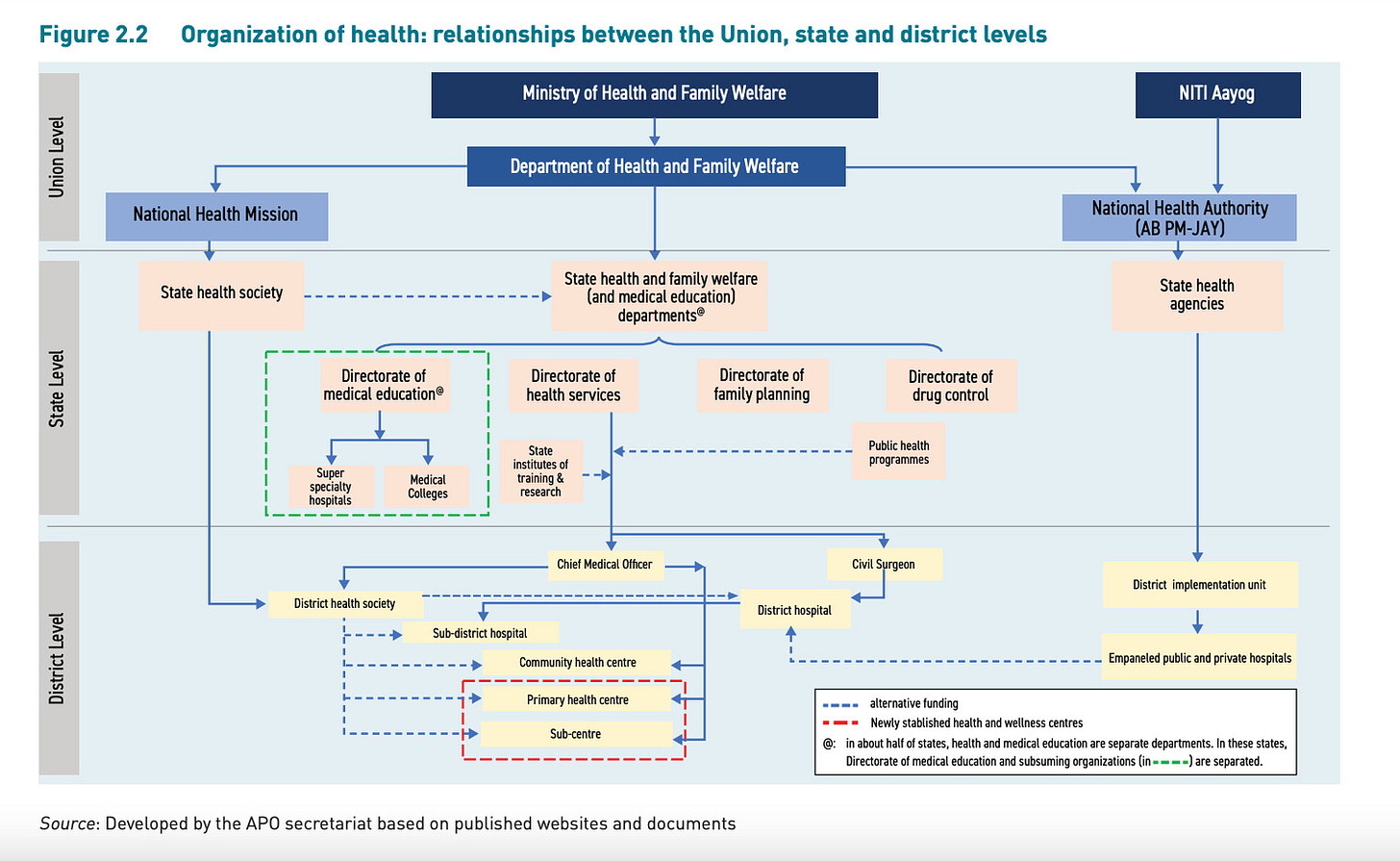
Here is a data-rich report explaining the state of the Indian rural infrastructure as of 2020 - 2021. The report states that “As of 31st March 2021, there are 156101 and 1718 Sub Centres (SC), 25140 and 5439 Primary Health Centres (PHCs) and 5481 and 470 Community Health Centres (CHCs) respectively, which are functioning in rural and urban areas of the country.” In addition to this three-tiered infra, the Medical Council of India (MCI) was also formed due to the Bhore Committee Report. The report recommended the establishment of a national body to regulate medical education and maintain standards of professional conduct among medical practitioners in India. This led to the formation of the Medical Council of India in 1934 under the Indian Medical Council Act. The MCI was responsible for recognising medical qualifications, maintaining a national register of medical practitioners, and regulating medical education and practice in India. However, the MCI was dissolved in 2018 and replaced with the National Medical Commission (NMC) as part of reforms to improve medical education and practice in India. Finally, the Ministry of Health and Family Planning was formed in 1955 due to the recommendations made by the Bhore Committee report. It was later renamed to the Ministry of Health and Family Welfare to reflect its expanded mandate.
The report’s recommendations have been used as a reference point for subsequent healthcare policy initiatives in India. The Bhore Committee Report laid the foundation for a more comprehensive and equitable healthcare system in the country, focusing on primary healthcare, preventive measures, and access to basic healthcare services. The report played a significant role in shaping the future of healthcare in India. Its recommendations continue to guide the country’s healthcare policies and remain a vital reference point for policymakers and healthcare professionals.
I would be remiss if I didn’t talk about one of the post-independence healthcare initiatives that put a dent in the Indian healthcare universe. Ayushman Bharat is a healthcare scheme launched by the Government of India in 2018. It put a dent because Pradhan Mantri Jan Arogya Yojana OR PMJAY (which operates under the Ayushman Bharat umbrella) provides free healthcare coverage up to INR 5 lakhs (~$7000) per family per year to over 100 million families (or about 500 million people) deemed socio-economically vulnerable. It is one of the world’s largest publicly funded health insurance schemes. The Government of India saw tangible benefits coming out of Ayushman Bharat. It doubled down on the initiative by complementing it with Ayushman Bharat Digital Mission (ABDM). Launched in 2021, ABDM is a digital health initiative to create a digital health ecosystem in the country. It aims to develop and implement digital health infrastructure, such as digital health IDs and registries, telemedicine services, and health information exchanges.
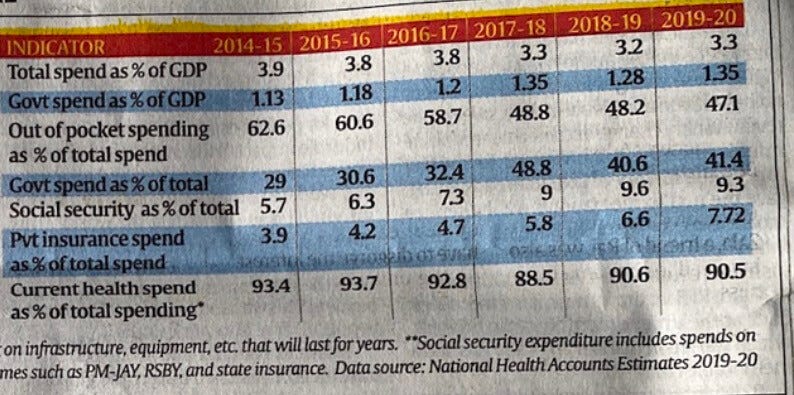
These initiatives have helped to improve the country's overall healthcare scenario. However, challenges persist. The shortage of healthcare professionals continues to be a significant issue, especially in rural areas. The quality of healthcare services remains a concern, with many hospitals needing more facilities and equipment. Additionally, the high cost of healthcare often prevents many people from accessing healthcare services. The various healthcare initiatives launched in India since independence have aimed to address the multiple challenges faced by the country's healthcare sector. While they have made significant progress, there is still a long way to go in improving healthcare infrastructure, increasing the number of healthcare professionals, and ensuring access to affordable and quality healthcare for all.
But with all its problems, the Indian Health System continues moving onward.
From Verandah Cases to Immaculate Verandahs: The Rise of the Indian Health System
I recently read an article in a national daily where a renowned neurologist from Pune recalls the state of Indian hospitals back in the day. He talks about how some patients used to be treated as ‘verandah cases’ due to a lack of equipment and testing. A ‘verandah case’ was where a patient was advised to be kept in the verandah (hallway) of the hospital because nothing much could be done. From then to now, almost every “verandah case” is treated, and patients are discharged in good health. This is not just luck.
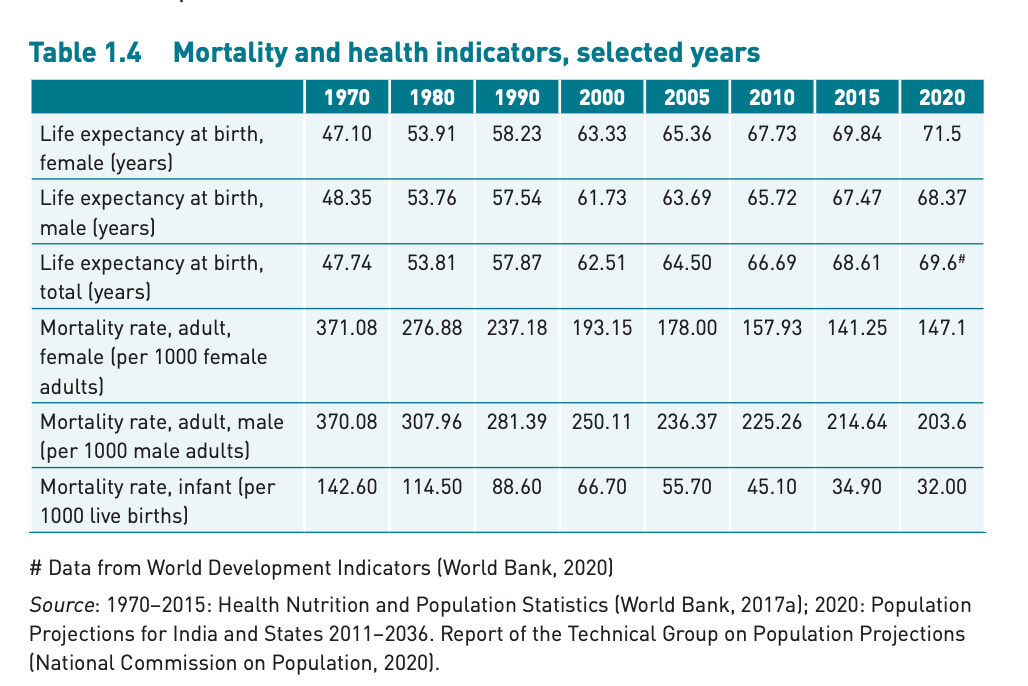
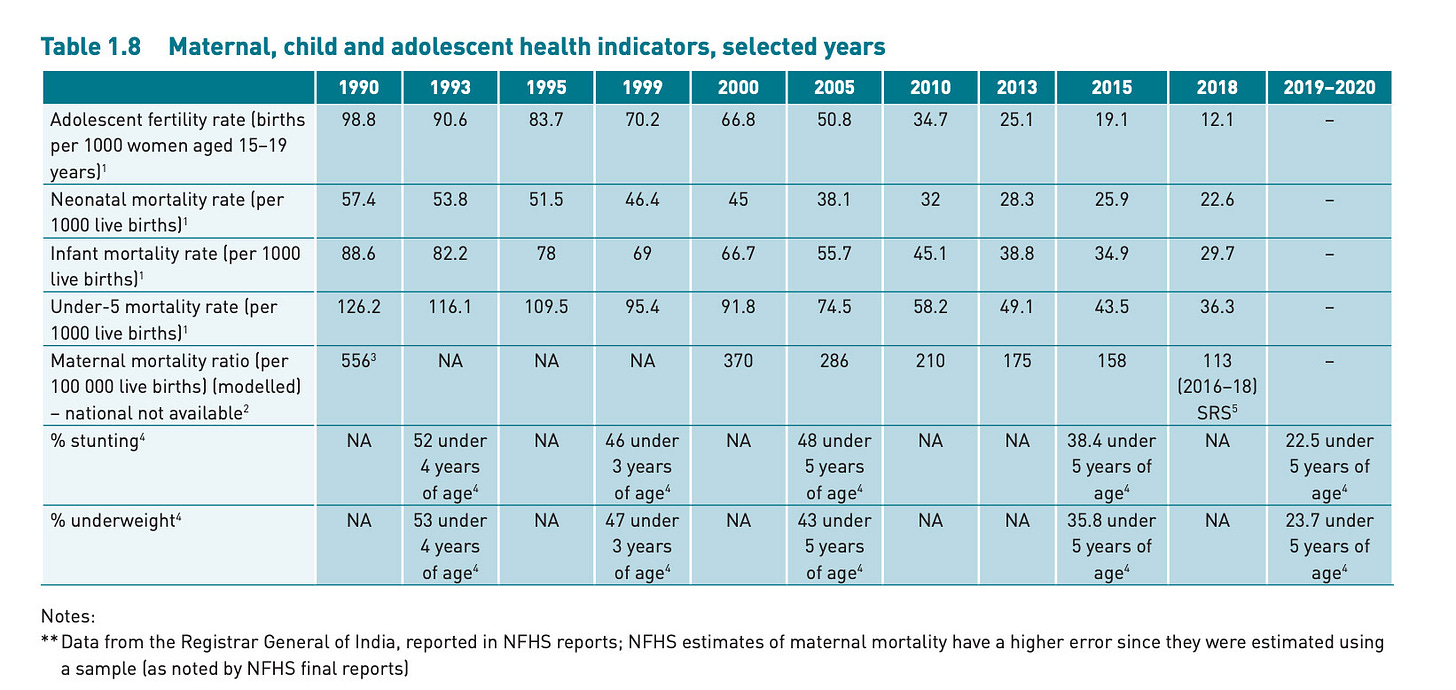
Former secretary in the Ministry of Health, Shailaja Chandra, writes in this aptly titled article ‘In Better Health’ how ‘the Indian health system has overcome seemingly unsurmountable problems, long considered hopeless.’ But whenever I read such statements, my mind goes looking for data. Because, as they say - In God we trust, everyone else has to bring data to the table. So, I dug out this 2022 report from the World Health Organization, which comprehensively assesses the state of the Indian Health System. The landing page says, ‘India has made significant improvements in the health outcomes of its people. Life expectancy at birth increased to 69.6 years in 2020 from an expected 47.7 years in 1970. MMR declined from 301 to 130 per 100 000 live births between 2003 and 2014-16, and IMR declined from 68 in 2000 to 24 per 1000 live births in 2016.’ Impressive.
You see, India is huge. It’s a federal union comprising 28 states and 8 union territories. It has over 4,000 cities, 718 districts, and 640,000 villages. Managing a large and complex health system has its own (humongous) challenges. It was very well the case in 1946 and is very much the case now. The only option in front of a country like India is to relentlessly pursue the goal of making Indians healthier.
India pursues this goal by having a laser focus on policy. In my experience as an Indian, we generally do not struggle at the policy level. Execution is the bottleneck.
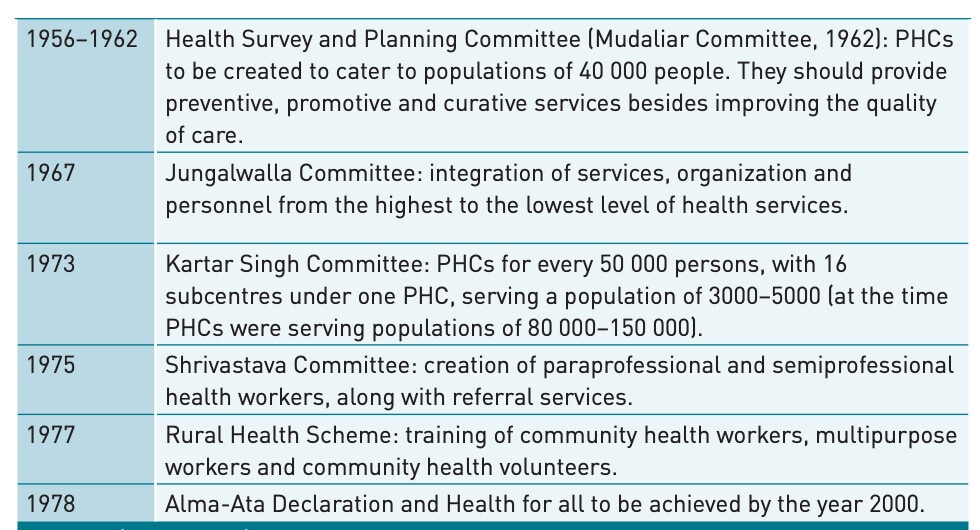
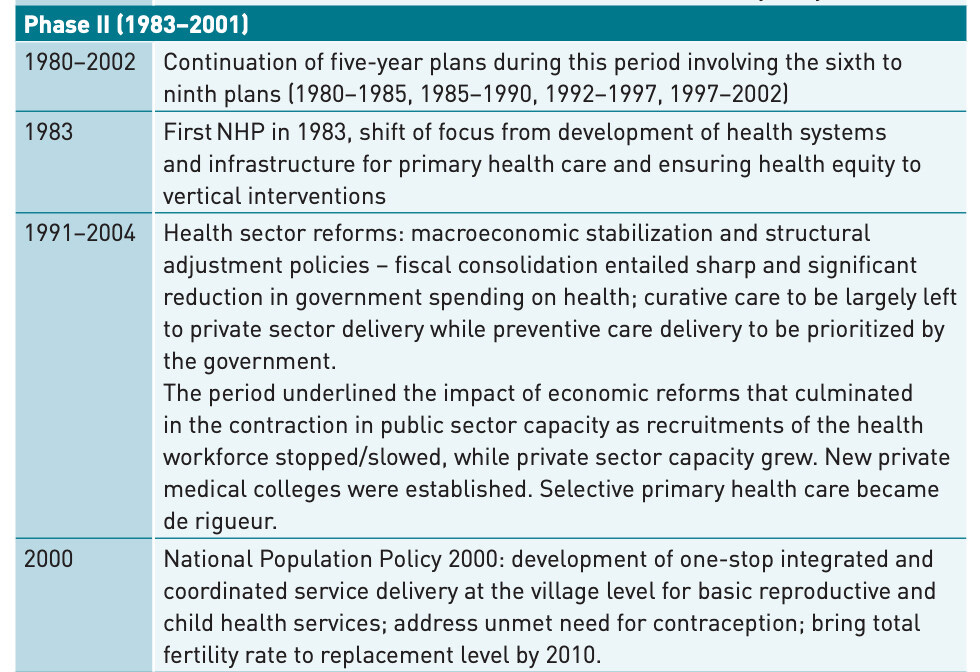
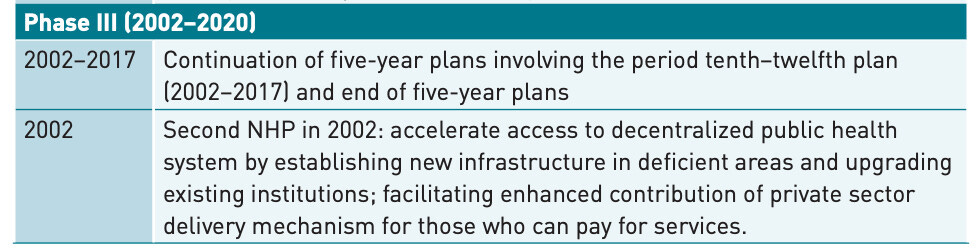
A case in point is that from 1946 through 2020, India has undergone numerous health policy reforms, which have set a strong foundation and pivoted as and when necessary.
The Indian government has already replaced the national health policy of 2002 with the one established in 2017
In March of 2021, the Indian government announced again that it would replace the National Health Policy 2017 with another new policy that is currently being developed. The new policy is expected to focus on the lessons learnt from the COVID-19 pandemic.
In February 2021, the Indian government announced merging the Ayushman Bharat scheme with the existing Rashtriya Swasthya Bima Yojana (RSBY) scheme. Ayushman Bharat was launched in 2018 as a flagship healthcare scheme to provide financial protection and healthcare services to the poorest sections of society. The merger is intended to streamline the delivery of healthcare services and reduce administrative costs.
In August 2019, the Indian government passed the National Medical Commission Bill, which replaced the Medical Council of India (MCI) with a new regulatory body called the National Medical Commission. The NMC was intended to streamline medical education and improve healthcare services in India. However, the bill was controversial and faced opposition from medical students and doctors, who argued that it would lead to the commercialisation of medical education and lower standards of care. In September 2020, the Indian government announced it would amend the NMC Bill to address some of these concerns.
The WHO publication on the Indian Health System beautifully segregates the last 7 decades of policies and critical reforms into 3 phases.
Phase 1
Phase 2
Phase 3
With a solid foundation of progressive policies in place, India's healthcare sector has embraced cutting-edge technologies to address the evolving needs of its population. One such transformative force is the advent of artificial intelligence (AI), which has been gaining momentum in Indian healthcare. By leveraging the power of AI, healthcare providers are revolutionising diagnostics, treatment protocols, and patient care delivery. Let's explore how AI is reshaping the landscape of Indian healthcare and driving significant improvements in quality, efficiency, and patient outcomes.
Ushering the Artificial Intelligence (AI) era in the Indian Healthcare
I was amazed to learn that the term ‘artificial intelligence’ was coined by John McCarthy of MIT as early as 1956 during the Dartmouth conference, which is widely considered the birthplace of AI. The obvious question remains - what took the world decades to adopt AI as we know it today? But that’s for another day. As for India, it is believed that AI entered India as early as 1960 through the work of Professor H.N. Mahabala at the Indian Institute of Technology, Kanpur. Fast forward to 2018, the Government of India made the evolution tangible by conceiving a national strategy on Artificial Intelligence. Healthcare is one of the five sectors envisioned to benefit the most from AI, specifically helping increase access and affordability of quality healthcare. All this got the ball rolling, and several healthcare startups emerged that used Artificial Intelligence to solve a market problem.
Niramai - uses AI to detect breast cancer at an early stage
Qure.ai - uses AI for radiology and pathology imaging analysis
Tricog Health - uses AI to diagnose heart diseases
SigTuple - uses AI for medical diagnostics
Mfine - uses AI to connect patients with doctors remotely
Practo - uses AI for appointment booking and management
Dozee - uses AI for remote monitoring of patient’s health
AI has the potential to revolutionise healthcare in India by improving access to quality care, reducing healthcare costs, and improving patient outcomes. However, ensuring that AI technologies are developed and deployed ethically and responsibly is crucial.
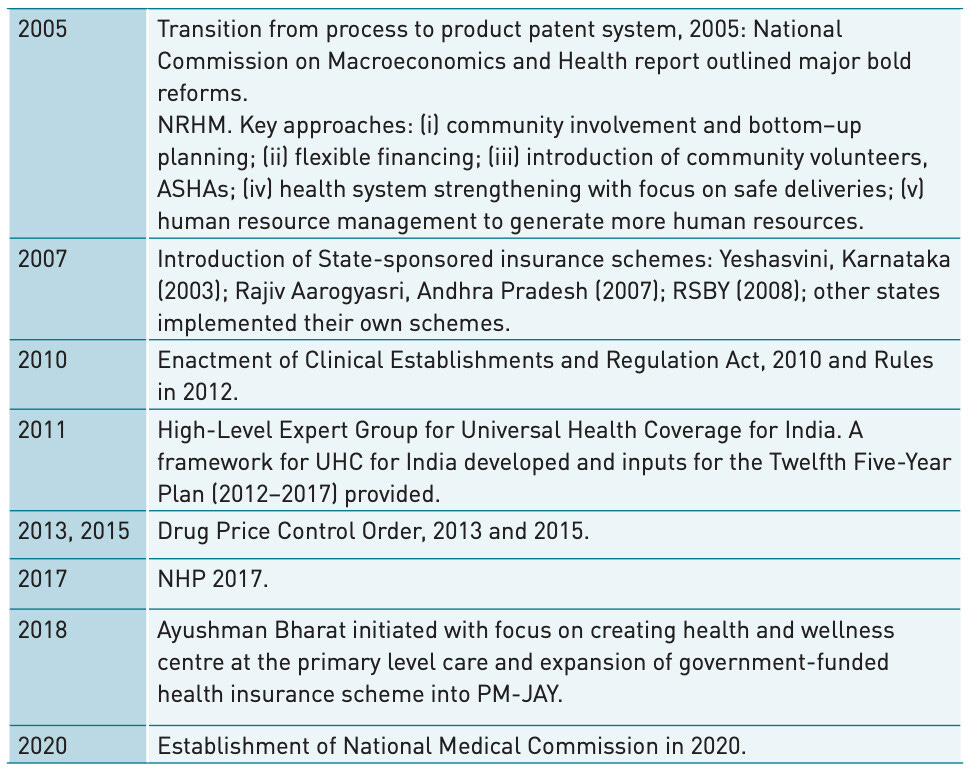
I read two pieces of information online that drove home the point of how quickly and elegantly India is embracing technology. In this article titled ‘India is Upgrading’, Nandan Nilekani argues that India is fast becoming an online, cashless, and high-productivity economy standing tall on the shoulders of its digital public infrastructure. This means something from the man who practically invented that digital public infrastructure.
Later in the day, I read an article about how a team of doctors in Delhi’s Safdarjung Hospital created a new world record by performing their 200th international live surgery using a Robot. Yes - “200th surgery using a ROBOT”.
"We performed very complex surgeries - Robotic partial nephrectomy in a very complex large hilar tumour in Chronic Kidney Disease patient. We were able to save the kidney and only removed the renal tumour. The second case was a 3-D Lap Bapro Flap for a long segment of uretic stricture. It was a complex reconstructive surgery, where also we were able to save the kidney successfully," said Dr Anup Kumar.
Now, I do not want to sound “artificially intelligent” by stating that I understand every word of what is written above. But that evening, I got a good night’s sleep with a generous appreciation of the fact that the Indian Health System has come a long way since our Rishis wrote those Vedas. I have no doubt that the Indian health system will continue to evolve, as it has for millennia and with all the excitement in the air, it still feels like Day 0.
Let’s get to work!
Reference
Supe, A. (2016). Evolution of medical education in India: The impact of colonialism. Journal of Postgraduate Medicine, 62(4), 255-259. https://doi.org/10.4103/0022-3859.191011
Selvaraj S, Karan K A, Srivastava S, Bhan N, & Mukhopadhyay I. India health system review. New Delhi: World Health Organization, Regional Office for South-East Asia; 2022.
Jaiswal, Y. S., & Williams, L. L. (2017). A glimpse of Ayurveda – The forgotten history and principles of Indian traditional medicine. Journal of Traditional and Complementary Medicine, 7(1), 50-53. https://doi.org/10.1016/j.jtcme.2016.02.002